Volume 18, Issue 4 (Jul-Aug 2024)
mljgoums 2024, 18(4): 14-16 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Subrat S, Prasad M L, Varshney K, Bansal K, Mahajan M, Chowdhury A. A study of prognostic significance of serum magnesium and serum potassium levels in acute stroke. mljgoums 2024; 18 (4) :14-16
URL: http://mlj.goums.ac.ir/article-1-1750-en.html
URL: http://mlj.goums.ac.ir/article-1-1750-en.html
Sudhanshu Subrat1 

 , Manohar Lal Prasad2
, Manohar Lal Prasad2 

 , Kavya Varshney3
, Kavya Varshney3 

 , Kanika Bansal4
, Kanika Bansal4 

 , Mayank Mahajan5
, Mayank Mahajan5 

 , Anindya Chowdhury1
, Anindya Chowdhury1 




 , Manohar Lal Prasad2
, Manohar Lal Prasad2 

 , Kavya Varshney3
, Kavya Varshney3 

 , Kanika Bansal4
, Kanika Bansal4 

 , Mayank Mahajan5
, Mayank Mahajan5 

 , Anindya Chowdhury1
, Anindya Chowdhury1 


1- Department of Medicine, MGM Medical College, Jamshedpur, India
2- Department of General Medicine, Rajendra Institute of Medical Sciences, Ranchi, India
3- Department of Lab Medicine, Delhi State Cancer Institute, Delhi, India ,kavyavarshney10@gmail.com
4- Department of Paediatrics, Lala Lajpat Rai Memorial Medical College, Meerut, India
5- Department of Medicine, Shaheed Nirmal Mahato Medical College and Hospital, Dhanbad, India
2- Department of General Medicine, Rajendra Institute of Medical Sciences, Ranchi, India
3- Department of Lab Medicine, Delhi State Cancer Institute, Delhi, India ,
4- Department of Paediatrics, Lala Lajpat Rai Memorial Medical College, Meerut, India
5- Department of Medicine, Shaheed Nirmal Mahato Medical College and Hospital, Dhanbad, India
Full-Text [PDF 313 kb]
(1043 Downloads)
| Abstract (HTML) (3822 Views)
Discussion
Stroke is an acute medical condition in which neuronal cell death is caused by poor blood flow to the brain, which may be due to an interruption of blood flow or the rupture of blood vessels inside the brain. When the blood supply to the brain is disrupted for a prolonged period, it leads to ischemia, initiating an ischemic cascade that further causes neuronal damage (11,12). It has been found that glutamate is one of the main culprits in excitotoxicity through its action on NMDA and AMPA receptors. Various studies have suggested the neuroprotective effects of magnesium and potassium ions through their influence on the glutamate receptor, endothelium, blood pressure reduction, anti-inflammatory and anti-apoptotic abilities, and inhibition of free radical injury (13-16).
In our study, we compared serum potassium and serum magnesium levels at admission with the GCS of patients at admission, as well as with the final neurological outcome during their hospital stay. The GCS is used to objectively describe the extent of impaired consciousness in all types of acute medical and trauma patients. The scale assesses patients based on eye-opening, motor, and verbal responses, indicating the patient’s state.
The mRS is a single-item, global outcome rating scale for patient’s post-stroke. It is used to categorize the level of functional independence with reference to pre-stroke activities rather than observed performance on a specific task (17). Its concurrent validity is demonstrated by a strong correlation with measures of stroke pathology and agreement with other stroke scales.
In the year 2017, Johnson et al. studied the correlation between serum potassium levels and the incidence of stroke, as well as mortality due to stroke, and found a significant correlation between them (18). In the same year, Kim et al. conducted a retrospective case-control study aimed at examining the effect of hypokalemia on the functional outcomes of patients with subacute stroke. For this study, a total of 96 post-stroke hemiplegic patients admitted to an inpatient clinic of the Department of Rehabilitation Medicine were recruited. They found that hypokalemia could be considered one of the deteriorating factors for post-stroke functional prognosis (19). A similar study was conducted by Patel et al. to assess serum magnesium levels in acute stroke and their correlation with neurological disability. They found a statistically significant correlation between the mRS score and serum magnesium levels, indicating that the severity of a stroke is inversely related to serum magnesium levels (20). In this study, we assessed the serum magnesium and potassium levels of stroke patients on their arrival and studied their correlation with the general condition of the patient on arrival as well as with the final neurological outcome. We found that GCS was lower at admission and mRS was higher at the time of discharge in patients with low serum magnesium and potassium levels at admission. This was consistent with the results of various previously available studies (18-20). We inferred that there was a significant correlation between serum magnesium and potassium levels with the initial condition of patients at presentation and also with morbidity and mortality in cases of acute stroke.
This study had some limitations. First, the sample size was only 150, so to confirm the association between serum potassium and magnesium with clinical outcomes, further studies need to be conducted with a larger sample size. Second, this study was conducted in a single center; therefore, multicenter-based studies are needed to confirm the association between serum potassium and magnesium with clinical outcomes in acute stroke in the general population. Third, there was a lack of proper extended follow-up.
Conclusion
Stroke is globally the second most common cause of death and disability after ischemic heart disease. The serum potassium and magnesium levels at admission in stroke patients had a significant correlation with the GCS of the patient at admission and with the mRS score at the time of discharge. Our study suggests a prognostic role of serum potassium and magnesium levels in patients with acute stroke. The lower the concentration of magnesium and potassium, the greater the magnitude of cerebral arterial contraction.
Acknowledgement
We acknowledge the support of the staff, faculty members, and all participants of the study.
Funding sources
None.
Ethical statement
Approval has been taken from the institutional ethical committee (Ethics code: 106IEC.RIMS).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author contributions
Sudhanshu Subrat contributed to study conception, material preparation, and data collection. Manohar Lal Prasad checked the manuscript. Kavya Varshney contributed to manuscript preparation and correspondence. Kanika Bansal contributed to study design and manuscript preparation. Mayank Mahajan contributed to data collection and analysis. Anindya Chowdhury contributed to data collection and interpretation. All authors read and approved the final manuscript.
Full-Text: (826 Views)
Introduction
The World Health Organization defines stroke as a rapidly developing clinical manifestation of focal or global disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than a vascular origin (1). Stroke is the second most common cause of death and disability worldwide after ischemic heart disease (2). It is the fifth leading cause of disability-adjusted life years in India (3). There were 6.5 million stroke cases in India, with an incidence of approximately 105-152 cases per one lakh population (4-6). In acute stroke, there is a rapid loss of brain potassium and magnesium levels, accompanied by the rapid uptake of sodium and calcium ions along with water. Magnesium and potassium also have a neuroprotective role through various mechanisms. Magnesium primarily acts via the N-methyl-D-aspartate (NMDA) receptor and helps regulate neuron hyperexcitability by modulating inhibitory GABA receptors. In cases of low Mg²⁺ concentration, the membrane potential becomes higher, relieving the Mg²⁺-mediated block of NMDA receptors and subsequently contributing to neuronal hyperexcitability. Mg²⁺ also plays a role in regulating the release of neuropeptides and oxidative stress, which significantly contribute to maintaining healthy neurological function. Potassium acts on cerebral arteries and increases the release of nitric oxide and prostacyclin, which in turn causes vasodilation and inhibits platelet aggregation. Potassium also reduces the formation of free radicals, thereby helping to minimize the extent of free radical-mediated injury in the setting of ischemic brain injury (7-9). Our aim was to study the prognostic significance of serum magnesium and potassium levels on clinical outcomes in patients admitted with acute stroke.
Methods
A hospital-based observational study was conducted at Rajendra Institute of Medical Sciences, Ranchi, over a period of 18 months after obtaining clearance from the institutional ethical committee. After obtaining consent, 150 patients with acute stroke of less than 72 hours' duration, aged 25 years and above, both male and female, were included in the study. Patients with end-stage renal disease, chronic diarrhea, regular alcohol intake, malabsorption syndrome, or a history of taking drugs causing hypokalemia and hypomagnesemia were excluded from the study.
After a detailed history, examination, and informed consent, 2 mL of venous blood was collected from the patient in a plain vial. Serum was separated by centrifugation, and magnesium and potassium levels were estimated using the colorimetric method. The cutoff for serum potassium levels was taken as 3.5 mEq/L (7,8) and for serum magnesium levels as 1.5 mg/dL, based on different studies (9,10). The neurological status of patients suffering from stroke was assessed using the Glasgow Coma Scale (GCS) at admission and the Modified Rankin Scale (mRS) at the time of discharge.
Statistical analysis was done using SPSS software version 27.0. Correlations between mRS and GCS with serum levels of magnesium and potassium were calculated using Spearman’s coefficient test. A p-value was calculated using an unpaired t-test, and p < 0.05 was considered statistically significant.
Results
To study the correlation between mRS and GCS scores with serum magnesium levels, two groups were made: one with a serum magnesium level <1.5 mg/dL and one with >1.5 mg/dL. The mean mRS and GCS in stroke cases with a serum magnesium level <1.5 mg/dL were 3.95 and 9.02, respectively. The mean mRS and GCS in stroke cases with a serum magnesium level >1.5 mg/dL were 3.56 and 9.69, respectively (Table 1). A positive correlation between mRS and GCS scores with serum magnesium levels was observed, which was statistically significant (p < 0.05) (Figure 1 and 2).
The World Health Organization defines stroke as a rapidly developing clinical manifestation of focal or global disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than a vascular origin (1). Stroke is the second most common cause of death and disability worldwide after ischemic heart disease (2). It is the fifth leading cause of disability-adjusted life years in India (3). There were 6.5 million stroke cases in India, with an incidence of approximately 105-152 cases per one lakh population (4-6). In acute stroke, there is a rapid loss of brain potassium and magnesium levels, accompanied by the rapid uptake of sodium and calcium ions along with water. Magnesium and potassium also have a neuroprotective role through various mechanisms. Magnesium primarily acts via the N-methyl-D-aspartate (NMDA) receptor and helps regulate neuron hyperexcitability by modulating inhibitory GABA receptors. In cases of low Mg²⁺ concentration, the membrane potential becomes higher, relieving the Mg²⁺-mediated block of NMDA receptors and subsequently contributing to neuronal hyperexcitability. Mg²⁺ also plays a role in regulating the release of neuropeptides and oxidative stress, which significantly contribute to maintaining healthy neurological function. Potassium acts on cerebral arteries and increases the release of nitric oxide and prostacyclin, which in turn causes vasodilation and inhibits platelet aggregation. Potassium also reduces the formation of free radicals, thereby helping to minimize the extent of free radical-mediated injury in the setting of ischemic brain injury (7-9). Our aim was to study the prognostic significance of serum magnesium and potassium levels on clinical outcomes in patients admitted with acute stroke.
Methods
A hospital-based observational study was conducted at Rajendra Institute of Medical Sciences, Ranchi, over a period of 18 months after obtaining clearance from the institutional ethical committee. After obtaining consent, 150 patients with acute stroke of less than 72 hours' duration, aged 25 years and above, both male and female, were included in the study. Patients with end-stage renal disease, chronic diarrhea, regular alcohol intake, malabsorption syndrome, or a history of taking drugs causing hypokalemia and hypomagnesemia were excluded from the study.
After a detailed history, examination, and informed consent, 2 mL of venous blood was collected from the patient in a plain vial. Serum was separated by centrifugation, and magnesium and potassium levels were estimated using the colorimetric method. The cutoff for serum potassium levels was taken as 3.5 mEq/L (7,8) and for serum magnesium levels as 1.5 mg/dL, based on different studies (9,10). The neurological status of patients suffering from stroke was assessed using the Glasgow Coma Scale (GCS) at admission and the Modified Rankin Scale (mRS) at the time of discharge.
Statistical analysis was done using SPSS software version 27.0. Correlations between mRS and GCS with serum levels of magnesium and potassium were calculated using Spearman’s coefficient test. A p-value was calculated using an unpaired t-test, and p < 0.05 was considered statistically significant.
Results
To study the correlation between mRS and GCS scores with serum magnesium levels, two groups were made: one with a serum magnesium level <1.5 mg/dL and one with >1.5 mg/dL. The mean mRS and GCS in stroke cases with a serum magnesium level <1.5 mg/dL were 3.95 and 9.02, respectively. The mean mRS and GCS in stroke cases with a serum magnesium level >1.5 mg/dL were 3.56 and 9.69, respectively (Table 1). A positive correlation between mRS and GCS scores with serum magnesium levels was observed, which was statistically significant (p < 0.05) (Figure 1 and 2).
|
Table 1. Correlation between mRS Score and GCS Score with serum magnesium and serum potassium levels (n = Number of participants)
.PNG) |
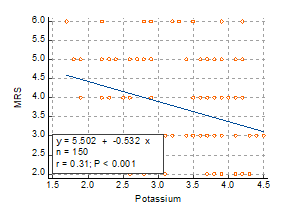
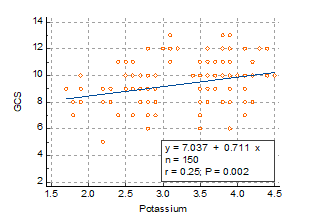
Similarly, to study the correlation between mRS and GCS scores with serum potassium levels, two groups were made: one with a serum potassium level < 3.5 mEq/L and one with > 3.5 mEq/L. The mean mRS and GCS in stroke patients with a serum potassium level < 3.5 mEq/L were 4.06 and 8.84, respectively. The mean mRS and GCS in stroke patients with a serum potassium level > 3.5 mEq/L were 3.47 and 9.84, respectively (Table 1). A positive correlation between mRS and GCS scores with serum potassium levels was observed, which was statistically significant (p < 0.05) (Figure 3 and 4). A statistically significant correlation was also observed between mRS and GCS in stroke patients with serum potassium and magnesium levels.
Discussion
Stroke is an acute medical condition in which neuronal cell death is caused by poor blood flow to the brain, which may be due to an interruption of blood flow or the rupture of blood vessels inside the brain. When the blood supply to the brain is disrupted for a prolonged period, it leads to ischemia, initiating an ischemic cascade that further causes neuronal damage (11,12). It has been found that glutamate is one of the main culprits in excitotoxicity through its action on NMDA and AMPA receptors. Various studies have suggested the neuroprotective effects of magnesium and potassium ions through their influence on the glutamate receptor, endothelium, blood pressure reduction, anti-inflammatory and anti-apoptotic abilities, and inhibition of free radical injury (13-16).
In our study, we compared serum potassium and serum magnesium levels at admission with the GCS of patients at admission, as well as with the final neurological outcome during their hospital stay. The GCS is used to objectively describe the extent of impaired consciousness in all types of acute medical and trauma patients. The scale assesses patients based on eye-opening, motor, and verbal responses, indicating the patient’s state.
The mRS is a single-item, global outcome rating scale for patient’s post-stroke. It is used to categorize the level of functional independence with reference to pre-stroke activities rather than observed performance on a specific task (17). Its concurrent validity is demonstrated by a strong correlation with measures of stroke pathology and agreement with other stroke scales.
In the year 2017, Johnson et al. studied the correlation between serum potassium levels and the incidence of stroke, as well as mortality due to stroke, and found a significant correlation between them (18). In the same year, Kim et al. conducted a retrospective case-control study aimed at examining the effect of hypokalemia on the functional outcomes of patients with subacute stroke. For this study, a total of 96 post-stroke hemiplegic patients admitted to an inpatient clinic of the Department of Rehabilitation Medicine were recruited. They found that hypokalemia could be considered one of the deteriorating factors for post-stroke functional prognosis (19). A similar study was conducted by Patel et al. to assess serum magnesium levels in acute stroke and their correlation with neurological disability. They found a statistically significant correlation between the mRS score and serum magnesium levels, indicating that the severity of a stroke is inversely related to serum magnesium levels (20). In this study, we assessed the serum magnesium and potassium levels of stroke patients on their arrival and studied their correlation with the general condition of the patient on arrival as well as with the final neurological outcome. We found that GCS was lower at admission and mRS was higher at the time of discharge in patients with low serum magnesium and potassium levels at admission. This was consistent with the results of various previously available studies (18-20). We inferred that there was a significant correlation between serum magnesium and potassium levels with the initial condition of patients at presentation and also with morbidity and mortality in cases of acute stroke.
This study had some limitations. First, the sample size was only 150, so to confirm the association between serum potassium and magnesium with clinical outcomes, further studies need to be conducted with a larger sample size. Second, this study was conducted in a single center; therefore, multicenter-based studies are needed to confirm the association between serum potassium and magnesium with clinical outcomes in acute stroke in the general population. Third, there was a lack of proper extended follow-up.
Conclusion
Stroke is globally the second most common cause of death and disability after ischemic heart disease. The serum potassium and magnesium levels at admission in stroke patients had a significant correlation with the GCS of the patient at admission and with the mRS score at the time of discharge. Our study suggests a prognostic role of serum potassium and magnesium levels in patients with acute stroke. The lower the concentration of magnesium and potassium, the greater the magnitude of cerebral arterial contraction.
Acknowledgement
We acknowledge the support of the staff, faculty members, and all participants of the study.
Funding sources
None.
Ethical statement
Approval has been taken from the institutional ethical committee (Ethics code: 106IEC.RIMS).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author contributions
Sudhanshu Subrat contributed to study conception, material preparation, and data collection. Manohar Lal Prasad checked the manuscript. Kavya Varshney contributed to manuscript preparation and correspondence. Kanika Bansal contributed to study design and manuscript preparation. Mayank Mahajan contributed to data collection and analysis. Anindya Chowdhury contributed to data collection and interpretation. All authors read and approved the final manuscript.
Research Article: Research Article |
Subject:
Laboratory Sciences
Received: 2023/11/26 | Accepted: 2024/08/28 | Published: 2025/03/11 | ePublished: 2025/03/11
Received: 2023/11/26 | Accepted: 2024/08/28 | Published: 2025/03/11 | ePublished: 2025/03/11
References
1. Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. 1980; 58: 113-130. [View at Publisher] [PMID] [Google Scholar]
2. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update from the GBD 2019 study. J Am Coll Cardiol. 2020; 76: 2982-3021. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Dandona L, Dandona R, Kumar GA, Shukla DK, Paul VK, Balakrishnan K, et al. Nations within a nation: Variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet. 2017; 390: 2437-60. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Prabhakaran D, Jeemon P, Sharma M, Roth GA, Johnson C, Harikrishnan S, et al. The changing patterns of cardiovascular diseases and their risk factors in the states of India: The Global Burden of Disease Study 1990-2016. Lancet Glob Health. 2018; 6: 1339-51. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global Burden of Diseases, Injuries, and Risk Factors Study 2010 (GBD 2010) and the GBD Stroke Experts Group. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014; 383(9913): 245-54. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021; 20(10): 795-820. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston: Butterworths; 1990. [View at Publisher] [PMID] [Google Scholar]
8. Castro D, Sharma S. Hypokalemia. 2025 Jan 19. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. [View at Publisher] [PMID]
9. Catalano A, Bellone F, Chilà D, Loddo S, Morabito N, Basile G, et al. Rates of hypomagnesemia and hypermagnesemia in medical settings. Magnes Res. 2021; 34(1): 1-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Daliparty, Vasudev Malik; Manu, Mohan K; Mohapatra, Aswini Kumar. Serum magnesium levels and its correlation with level of control in patients with asthma: A hospital-based, cross-sectional, prospective study. Lung India. 2018; 35(5 ): 407-10. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Musuka TD, Wilton SB, Traboulsi M, Hill MD. Diagnosis and management of acute ischemic stroke: speed is critical. CMAJ. 2015; 187(12): 887-93. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Kuriakose D, Xiao Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int J Mol Sci. 2020; 21(20): 7609. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Touyz RM. Magnesium supplementation as an adjuvant to synthetic calcium channel antagonists in the treatment of hypertension. Med Hypotheses. 1991; 36(2): 140-1. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Altura BM, Altura BT. New perspectives on the role of magnesium in the pathophysiology of the cardiovascular system. I. Clinical aspects. Magnesium. 1985; 4: 226-244. [View at Publisher] [PMID] [Google Scholar]
15. Haddy FJ, Vanhoutte PM, Feletou M. Role of potassium in regulating blood flow and blood pressure. Am J Physiol Regul Integr Comp Physiol. 2006; 290(3): R546-52. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. McCabe RD, Bakarich MA, Srivastava K, Young DB. Potassium inhibits free radical formation. Hypertension. 1994;24(1):77-82. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Shinohara, Y., Minematsu, K., Amano, T., Ohashi, Y. Modified Rankin Scale with expanded guidance scheme and interview questionnaire: interrater Agreement and Reproducibility of Assessment. Cerebrovasc Dis. 2006; 21: 271-27. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Johnson LS, Mattsson N, Sajadieh A, Wollmer P, Söderholm M. Serum Potassium Is Positively Associated With Stroke and Mortality in the Large, Population-Based Malmö Preventive Project Cohort. Stroke. 2017;48(11):2973-2978. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Young Seok Kim , Yoon Ghil Park , Jinyoung Park , Hosung Yi , Eu Jeong Ko. Significance of Hypokalemia in Functional Outcomes of Patients with Subacute Stroke. 2019;12(2):e13 [View at Publisher] [DOI] [Google Scholar]
20. Patel RK, Sahu D, Gupta S. Assessment of Serum Magnesium Levels in Stroke Patients and its Correlation with Severity of Neurological Disability. IJCMR. 2018. [View at Publisher] [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




.PNG)
.PNG)


 goums.ac.ir
goums.ac.ir yahoo.com
yahoo.com