Volume 18, Issue 3 (May-Jun 2024)
mljgoums 2024, 18(3): 13-15 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Michel T, Esther V, Bernard B, Louise M N, Simon Stevensen S, Raissa N et al . Chemiluminescence vs hemagglutination assay in the detection of Anti-Treponema pallidum antibodies. mljgoums 2024; 18 (3) :13-15
URL: http://mlj.goums.ac.ir/article-1-1590-en.html
URL: http://mlj.goums.ac.ir/article-1-1590-en.html
Toukam Michel1 

 , Voundi-Voundi Esther2
, Voundi-Voundi Esther2 

 , Bole Bernard3
, Bole Bernard3 
 , Mviena Nyimbe Louise4
, Mviena Nyimbe Louise4 
 , Sahmo Simon Stevensen4
, Sahmo Simon Stevensen4 
 , Nogue Raissa4
, Nogue Raissa4 
 , Kasia Jean Marie5
, Kasia Jean Marie5 



 , Voundi-Voundi Esther2
, Voundi-Voundi Esther2 

 , Bole Bernard3
, Bole Bernard3 
 , Mviena Nyimbe Louise4
, Mviena Nyimbe Louise4 
 , Sahmo Simon Stevensen4
, Sahmo Simon Stevensen4 
 , Nogue Raissa4
, Nogue Raissa4 
 , Kasia Jean Marie5
, Kasia Jean Marie5 

1- Department of Microbiology, Parasitology, Hematology and infectious diseases, Faculty of Medicine and Biomedical Sciences, The University of Yaoundé I, Cameroon , mtoukam2002@gmail.com
2- Department of Microbiology, Parasitology, Hematology and infectious diseases, Faculty of Medicine and Biomedical Sciences, The University of Yaoundé I, Cameroon
3- Ministry of Public Health, Cameroon
4- Gynaecological Endoscopic Surgery and Human Reproductive Teaching Hospital, Cameroon
5- Faculty of Medicine and Biomedical Sciences, The University of Yaoundé I, Cameroon
2- Department of Microbiology, Parasitology, Hematology and infectious diseases, Faculty of Medicine and Biomedical Sciences, The University of Yaoundé I, Cameroon
3- Ministry of Public Health, Cameroon
4- Gynaecological Endoscopic Surgery and Human Reproductive Teaching Hospital, Cameroon
5- Faculty of Medicine and Biomedical Sciences, The University of Yaoundé I, Cameroon
Full-Text [PDF 334 kb]
(1135 Downloads)
| Abstract (HTML) (4111 Views)
Full-Text: (1005 Views)
Introduction
According to the World Health Organization (WHO), every year, 357 million people worldwide contract one of the four sexually transmitted infections (STIs): chlamydia, gonorrhea, syphilis, or trichomoniasis (1). These infections can have serious consequences for reproductive health, including infertility and mother-to-child transmission (1). Among these STIs, syphilis, known as the "great simulator," had almost disappeared following the use of penicillin but has been resurgent since 2000 (2). Since then, the WHO estimates that 5.6 million people are infected with Treponema pallidum each year (1), with sub-Saharan Africa having by far the highest regional prevalence (3). Early detection and treatment of syphilis are crucial for preventing late complications in the infected person and transmission to sexual partners (4). However, syphilis poses a diagnostic problem because Treponema pallidum, the causative agent of this infection, is not cultivable in vitro (5). Reliable diagnostic tests are widely used in high-income countries but are rarely available in low- and middle-income countries (1). In our context, the commonly used test for anti-treponemal antibodies is the Treponema pallidum hemagglutination assay (TPHA). This assay can yield false-negative results in individuals tested during primary syphilis and false-positive results associated with various medical conditions (6). Other methods for the diagnosis of syphilis, such as chemiluminescence, are also available. The results of the evaluation of this technique are contradictory in the literature. Some studies show that chemiluminescence is less sensitive and specific than other techniques for detecting anti-Treponema pallidum antibodies (7-9), while others indicate that it is more sensitive and specific (10-12). In addition, some studies show that the performance of chemiluminescence is influenced by certain factors (12,13). The general objective of our study was to compare chemiluminescence and hemagglutination assays in detecting anti-Treponema pallidum antibodies in our context.
Methods
We conducted a cross-sectional, analytical, and comparative study at the Gynaecological Endoscopic Surgery and Human Reproductive Teaching Hospital (GESHRTH). This study was conducted from November 1, 2018, to April 1, 2019, for a total duration of 6 months.
The blood samples were taken from couples being followed for infertility, a population with a high prevalence of STIs that may be the cause of their infertility.
The participants signed an informed consent form and then completed a questionnaire including sociodemographic data. Subsequently, 10 ml of blood were collected in sterile, pre-labeled tubes under aseptic conditions. The blood was processed, and the serum was decanted into cryotubes and stored in a freezer at -20°C. Hemagglutination assay, chemiluminescence assay, and immunoblot tests were performed in the GESHRTH laboratory. All discordant sera, as well as 20 negative and 20 positive sera for the two tests, were sent to the CERBA laboratory in Saint-Ouen-l'Aumône (France) for immunoblot testing (For anti-Treponema pallidum IgG and IgM antibodies). The study population was predominantly female, with a sex ratio of 0.83. The most represented age group was 25-35 years (252; 42.0%).
The TPHA is an indirect hemagglutination test for the determination of Treponema pallidum antibodies in human serum or plasma. Stabilized avian erythrocytes are sensitized with antigenic components of pathogenic Treponema pallidum (Nichol's strain). These "test" cells agglutinate in the presence of Treponema pallidum-specific antibodies and form a characteristic image (Haze) in the wells of a microtiter plate. Any non-specific reaction is detected using "Control" cells, which are non-sensitized avian erythrocytes. Non-pathogenic treponemal antibodies are absorbed by Reiter's treponemal extract, included in the test cell suspension. The test result is obtained within 45 to 60 minutes. At this time, the characteristic haze of cell agglutination is easily readable and persistent (1). Indeterminate results, as well as positives, were retested in a double-blind fashion.
Chemiluminescence was performed using the COBAS e 411, a fully automated analyzer employing patented electrogenerated chemiluminescence technology for immunoassay. It is designed for the quantitative and qualitative determination of in vitro assays for a wide range of applications, including infectious diseases. For detecting anti-Treponema pallidum antibodies, it is a one-step dual antigen sandwich assay. The assay detects total IgG and IgM antibodies to bacterial TpN15, TpN17, and TpN47.
The Western blot (Protein blot or immunoblot) is a rapid and sensitive test for the detection and characterization of proteins. It is based on the principle of immunochromatography, in which proteins are separated in polyacrylamide gel according to their molecular weight. The separated proteins are then transferred or electrotransferred onto a nitrocellulose membrane and are detected using an antibody and a substrate labeled with a primary antibody and a secondary enzyme.
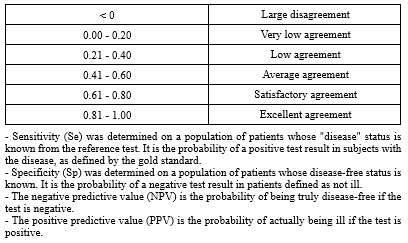
The data obtained were entered and recorded using Excel and Word software, and were analyzed using IBM-SPSS version 24 software for Windows with a statistically significant value set at p<0.05. Qualitative data will be expressed in terms of numbers and frequency. Quantitative data will be represented by their mean (± standard deviation) or median (Interquartile range), depending on the type of distribution. The following performance parameters were determined: The agreement was determined by Cohen's kappa coefficient (Table 1).
To carry out this work, we obtained administrative authorization for research from the GESHRTH and ethical clearance from the Institutional Research Ethics Committee of the Faculty of Medicine and Biomedical Sciences of the University of Yaoundé I. The information collected was used exclusively within the framework of this study and in strict compliance with medical confidentiality. The screening tests were performed free of charge for the participants.
Results
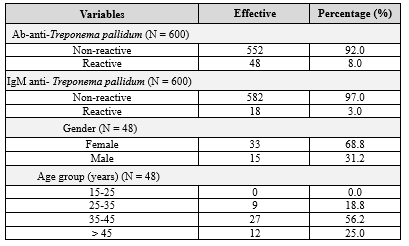
After serological testing, 48 participants tested positive for either IgG and/or IgM, resulting in an exposure prevalence of 8.0%. Moreover, 18 samples were positive for IgM, indicating a syphilis prevalence of 3.0%. Women were the most represented group, with 33 (68.8%) cases. The age group most commonly found was 35-45 years (27/48; 56.3%) (Table 2).
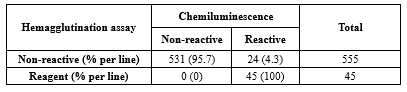
All 45 samples reactive by the hemagglutination assay were also reactive by chemiluminescence, resulting in 100% agreement. However, 555 samples were non-reactive by hemagglutination, while chemiluminescence identified 531 of these as non-reactive, resulting in 24 mismatches, or 95.7% agreement. Therefore, the Kappa agreement of 0.768 falls between 0.61 and 0.80, indicating significantly satisfactory agreement (p<0.0001) (Table 3).
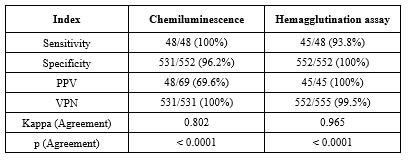
The sensitivity and specificity of chemiluminescence were higher (100% and 100%, respectively) compared to hemagglutination (93.8% and 96.2%, respectively). The PPV was higher with hemagglutination (100%) than with chemiluminescence (69.6%), while the NPVs were almost identical for chemiluminescence (100%) and hemagglutination (99.5%). Cohen's kappa agreements between chemiluminescence/immunoblot and hemagglutination /immunoblot were greater than 0.8, indicating excellent agreement with the reference test (p<0.0001) (Table 4).
Discussion
Our study compared chemiluminescence and hemagglutination assays for detecting anti-Treponema pallidum antibodies. Results showed that chemiluminescence is more sensitive but less specific than hemagglutination. The prevalence of syphilis was 3%, and the prevalence of exposure was 8%. The participants were predominantly female (54.5%). Since our population consisted of individuals being followed for infertility, the predominance of females may be due to the ostracism of women in cases where a child is desired in a couple. The seroprevalence of syphilis in our sample was 3%, differing from the findings of Jary et al. (14) and Koksal et al. (15), who respectively reported prevalences of 0.04% and 19.3%. These disparate prevalences could be due to the different methodologies used. Indeed, Jary et al. worked on the seroprevalence among blood donors, while Koksal et al. studied men with HIV. Blood donors are generally volunteers in apparent good health, and initial medical screening eliminates those with a risk of STIs upon interrogation. This would explain the low prevalence in this population. On the other hand, people living with HIV, due to similar modes of transmission, have an increased risk of contracting other STIs such as syphilis; hence, the prevalence is high in this population. For our target population, the prevalence was not very high in patients followed for couple infertility, where STIs are a main cause in our context. However, the data highlighted the non-negligible impact of syphilis on couple fertility, as indicated by the exposure prevalence of 8.0% defined by the presence of IgG anti-Treponema pallidum. To compare chemiluminescence and hemagglutination, we used immunoblot as a reference test. We evaluated the intrinsic characteristics of chemiluminescence, including sensitivity and specificity, as well as its extrinsic characteristics, including predictive values and concordance. The sensitivity and specificity of chemiluminescence were 100% and 96.2%, respectively. In the study by Wang et al., this sensitivity is identical to ours, but the specificity is greater (99.6%) (13). This difference may be attributed to factors such as sex, pregnancy, history of syphilis, and other STIs, as found by Bopage et al. in their study in Australia (12). Comparing the two techniques, we noted that the sensitivity of chemiluminescence was higher than that of hemagglutination (100% vs. 93.8%). Moreover, the specificity of hemagglutination was higher than that of chemiluminescence (100% vs. 96.2%). The PPV was higher with hemagglutination than with chemiluminescence (100% vs. 69.6%), while the NPVs were almost identical between the two techniques. With excellent agreement between the two techniques and the reference test, these tests provide comparable results and could be considered in a diagnostic algorithm in our context.
Conclusion
The prevalence of syphilis and the prevalence of exposure to syphilis are not negligible in infertile couples. Both hemagglutination and chemiluminescence demonstrated good performance for detecting anti-Treponema pallidum antibodies, in accordance with the WHO standards. Chemiluminescence had better sensitivity than plate hemagglutination for detecting anti-Treponema pallidum antibodies but lower specificity compared to hemagglutination.
Acknowledgement
The research team would like to thank all the participants in this study.
Funding sources
The authors of this article did not receive any financial support for the research.
Ethical statement
This study has been approved by the Ethics Committee of the Gynaecological Endoscopic Surgery and Human Reproductive Teaching Hospital (GESHRTH).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author contributions
All authors have contributed equally.
According to the World Health Organization (WHO), every year, 357 million people worldwide contract one of the four sexually transmitted infections (STIs): chlamydia, gonorrhea, syphilis, or trichomoniasis (1). These infections can have serious consequences for reproductive health, including infertility and mother-to-child transmission (1). Among these STIs, syphilis, known as the "great simulator," had almost disappeared following the use of penicillin but has been resurgent since 2000 (2). Since then, the WHO estimates that 5.6 million people are infected with Treponema pallidum each year (1), with sub-Saharan Africa having by far the highest regional prevalence (3). Early detection and treatment of syphilis are crucial for preventing late complications in the infected person and transmission to sexual partners (4). However, syphilis poses a diagnostic problem because Treponema pallidum, the causative agent of this infection, is not cultivable in vitro (5). Reliable diagnostic tests are widely used in high-income countries but are rarely available in low- and middle-income countries (1). In our context, the commonly used test for anti-treponemal antibodies is the Treponema pallidum hemagglutination assay (TPHA). This assay can yield false-negative results in individuals tested during primary syphilis and false-positive results associated with various medical conditions (6). Other methods for the diagnosis of syphilis, such as chemiluminescence, are also available. The results of the evaluation of this technique are contradictory in the literature. Some studies show that chemiluminescence is less sensitive and specific than other techniques for detecting anti-Treponema pallidum antibodies (7-9), while others indicate that it is more sensitive and specific (10-12). In addition, some studies show that the performance of chemiluminescence is influenced by certain factors (12,13). The general objective of our study was to compare chemiluminescence and hemagglutination assays in detecting anti-Treponema pallidum antibodies in our context.
Methods
We conducted a cross-sectional, analytical, and comparative study at the Gynaecological Endoscopic Surgery and Human Reproductive Teaching Hospital (GESHRTH). This study was conducted from November 1, 2018, to April 1, 2019, for a total duration of 6 months.
The blood samples were taken from couples being followed for infertility, a population with a high prevalence of STIs that may be the cause of their infertility.
The participants signed an informed consent form and then completed a questionnaire including sociodemographic data. Subsequently, 10 ml of blood were collected in sterile, pre-labeled tubes under aseptic conditions. The blood was processed, and the serum was decanted into cryotubes and stored in a freezer at -20°C. Hemagglutination assay, chemiluminescence assay, and immunoblot tests were performed in the GESHRTH laboratory. All discordant sera, as well as 20 negative and 20 positive sera for the two tests, were sent to the CERBA laboratory in Saint-Ouen-l'Aumône (France) for immunoblot testing (For anti-Treponema pallidum IgG and IgM antibodies). The study population was predominantly female, with a sex ratio of 0.83. The most represented age group was 25-35 years (252; 42.0%).
The TPHA is an indirect hemagglutination test for the determination of Treponema pallidum antibodies in human serum or plasma. Stabilized avian erythrocytes are sensitized with antigenic components of pathogenic Treponema pallidum (Nichol's strain). These "test" cells agglutinate in the presence of Treponema pallidum-specific antibodies and form a characteristic image (Haze) in the wells of a microtiter plate. Any non-specific reaction is detected using "Control" cells, which are non-sensitized avian erythrocytes. Non-pathogenic treponemal antibodies are absorbed by Reiter's treponemal extract, included in the test cell suspension. The test result is obtained within 45 to 60 minutes. At this time, the characteristic haze of cell agglutination is easily readable and persistent (1). Indeterminate results, as well as positives, were retested in a double-blind fashion.
Chemiluminescence was performed using the COBAS e 411, a fully automated analyzer employing patented electrogenerated chemiluminescence technology for immunoassay. It is designed for the quantitative and qualitative determination of in vitro assays for a wide range of applications, including infectious diseases. For detecting anti-Treponema pallidum antibodies, it is a one-step dual antigen sandwich assay. The assay detects total IgG and IgM antibodies to bacterial TpN15, TpN17, and TpN47.
The Western blot (Protein blot or immunoblot) is a rapid and sensitive test for the detection and characterization of proteins. It is based on the principle of immunochromatography, in which proteins are separated in polyacrylamide gel according to their molecular weight. The separated proteins are then transferred or electrotransferred onto a nitrocellulose membrane and are detected using an antibody and a substrate labeled with a primary antibody and a secondary enzyme.
The data obtained were entered and recorded using Excel and Word software, and were analyzed using IBM-SPSS version 24 software for Windows with a statistically significant value set at p<0.05. Qualitative data will be expressed in terms of numbers and frequency. Quantitative data will be represented by their mean (± standard deviation) or median (Interquartile range), depending on the type of distribution. The following performance parameters were determined: The agreement was determined by Cohen's kappa coefficient (Table 1).
Results
After serological testing, 48 participants tested positive for either IgG and/or IgM, resulting in an exposure prevalence of 8.0%. Moreover, 18 samples were positive for IgM, indicating a syphilis prevalence of 3.0%. Women were the most represented group, with 33 (68.8%) cases. The age group most commonly found was 35-45 years (27/48; 56.3%) (Table 2).
|
Table 2. Distribution of Treponema Pallidum
 |
|
Table 3. Agreement measure between chemiluminescence and hemagglutination assay
 |
|
Table 4. Comparison of the tests according to the reference test
 |
Discussion
Our study compared chemiluminescence and hemagglutination assays for detecting anti-Treponema pallidum antibodies. Results showed that chemiluminescence is more sensitive but less specific than hemagglutination. The prevalence of syphilis was 3%, and the prevalence of exposure was 8%. The participants were predominantly female (54.5%). Since our population consisted of individuals being followed for infertility, the predominance of females may be due to the ostracism of women in cases where a child is desired in a couple. The seroprevalence of syphilis in our sample was 3%, differing from the findings of Jary et al. (14) and Koksal et al. (15), who respectively reported prevalences of 0.04% and 19.3%. These disparate prevalences could be due to the different methodologies used. Indeed, Jary et al. worked on the seroprevalence among blood donors, while Koksal et al. studied men with HIV. Blood donors are generally volunteers in apparent good health, and initial medical screening eliminates those with a risk of STIs upon interrogation. This would explain the low prevalence in this population. On the other hand, people living with HIV, due to similar modes of transmission, have an increased risk of contracting other STIs such as syphilis; hence, the prevalence is high in this population. For our target population, the prevalence was not very high in patients followed for couple infertility, where STIs are a main cause in our context. However, the data highlighted the non-negligible impact of syphilis on couple fertility, as indicated by the exposure prevalence of 8.0% defined by the presence of IgG anti-Treponema pallidum. To compare chemiluminescence and hemagglutination, we used immunoblot as a reference test. We evaluated the intrinsic characteristics of chemiluminescence, including sensitivity and specificity, as well as its extrinsic characteristics, including predictive values and concordance. The sensitivity and specificity of chemiluminescence were 100% and 96.2%, respectively. In the study by Wang et al., this sensitivity is identical to ours, but the specificity is greater (99.6%) (13). This difference may be attributed to factors such as sex, pregnancy, history of syphilis, and other STIs, as found by Bopage et al. in their study in Australia (12). Comparing the two techniques, we noted that the sensitivity of chemiluminescence was higher than that of hemagglutination (100% vs. 93.8%). Moreover, the specificity of hemagglutination was higher than that of chemiluminescence (100% vs. 96.2%). The PPV was higher with hemagglutination than with chemiluminescence (100% vs. 69.6%), while the NPVs were almost identical between the two techniques. With excellent agreement between the two techniques and the reference test, these tests provide comparable results and could be considered in a diagnostic algorithm in our context.
Conclusion
The prevalence of syphilis and the prevalence of exposure to syphilis are not negligible in infertile couples. Both hemagglutination and chemiluminescence demonstrated good performance for detecting anti-Treponema pallidum antibodies, in accordance with the WHO standards. Chemiluminescence had better sensitivity than plate hemagglutination for detecting anti-Treponema pallidum antibodies but lower specificity compared to hemagglutination.
Acknowledgement
The research team would like to thank all the participants in this study.
Funding sources
The authors of this article did not receive any financial support for the research.
Ethical statement
This study has been approved by the Ethics Committee of the Gynaecological Endoscopic Surgery and Human Reproductive Teaching Hospital (GESHRTH).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author contributions
All authors have contributed equally.
Research Article: Research Article |
Subject:
Laboratory Sciences
Received: 2022/10/28 | Accepted: 2024/01/21 | Published: 2024/11/12 | ePublished: 2024/11/12
Received: 2022/10/28 | Accepted: 2024/01/21 | Published: 2024/11/12 | ePublished: 2024/11/12
References
1. WHO. Sexually transmitted infections. 2023. [View at Publisher]
2. Buder S, Schöfer H, Meyer T, Bremer V, Kohl PK, Skaletz-Rorowski A, et al. Bacterial sexually transmitted infections. J Dtsch Dermatol Ges. 2019; 17(3): 287-315. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. McClintock HF, Dulak SL. Intimate partner violence and Sexually Transmitted Infections among women in Sub-Saharan Africa. J Immigr Minor Health. 2021; 23(2): 191-198. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. WHO. Rapid Syphilis Tests - IRIS. 2019. [View at Publisher]
5. Guntz Ph, North ML. Sérodiagnostic de la syphilis. Rev Francoph Lab. 1997;1997(294):51-8. [View at Publisher] [DOI] [Google Scholar]
6. Matthias J, Klingler EJ, Schillinger JA, Keller G, Wilson C, Peterman TA. Frequency and characteristics of biological false-positive test results for syphilis reported in Florida and New York City, USA, 2013 to 2017. Journal of Clinical Microbiology. 2019; 57(11): e00898-19. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Tao C, Hao X, Xu W, Zhang J, Pan S, Tao Z, et al. Evaluation of the Elecsys syphilis immunoassay for routine screening of serum samples in China. Sci Rep. 2017; 7(1): 9559. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Li Z, Feng Z, Liu P, Yan C. Screening for antibodies against Treponema pallidum with chemiluminescent microparticle immunoassay: analysis of discordant serology results and clinical characterization. Ann Clin Biochem. 2016; 53(5): 588 92. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Zhiyan L, Meiling W, Ping L, Jinhua D, Zhenlin Y, Zhenru F. Consistency Between Treponema pallidum Particle Agglutination Assay and Architect Chemiluminescent Microparticle Immunoassay and Characterization of Inconsistent Samples. J Clin Lab Anal. 2015; 29(4): 281 4. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Mo X, Jin Y, Yang Y, Hu W, Gu W. Evaluation of a new chemiluminescence immunoassay for diagnosis of syphilis. Eur J Med Res. 2010; 15(2): 66 9. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Chen Q, An J, Rao C, Wang T, Li D, Feng S, Tao C. Performance Evaluation of a Novel Chemiluminescence Assay Detecting Treponema Pallidum Antibody as a Syphilis Screening Method. Clin Lab. 2016; 62(4): 519-26. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Bopage RI, Vollmer-Conna U, Shand AW, Post JJ. Sex differences in the significance of isolated reactive treponemal chemiluminescence immunoassay results. Sex Transm Infect. 2018; 94(3): 187 91. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Wang K-D, Xu D-J, Su J-R. Preferable procedure for the screening of syphilis in clinical laboratories in China. Infect Dis (Lond). 2016; 48(1): 26 31. [View at Publisher] [DOI]
14. Jary A, Dienta S, Leducq V, Le Hingrat Q, Cisse M, Diarra AB, et al. Seroprevalence and risk factors for HIV, HCV, HBV and syphilis among blood donors in Mali. BMC Infect Dis. 2019; 19(1): 1064. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Köksal MO, Beka H, Evlice O, Çiftçi S, Keskin F, Başaran S, et al. Syphilis seroprevalence among HIV-infected males in Istanbul, Turkey. Rev Argent Microbiol. 2020; 52(4): 266-271. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





 goums.ac.ir
goums.ac.ir yahoo.com
yahoo.com