Volume 18, Issue 1 (Jan-Feb 2024)
mljgoums 2024, 18(1): 4-8 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jan I, Eachkoti R, Farooq I, Farooq S, Saleem S, Majid S. D-NLR, and neutrophil count as early predictive biomarkers of disease severity and poor disease outcome in SARS-CoV-2 infected patients from Kashmir. mljgoums 2024; 18 (1) :4-8
URL: http://mlj.goums.ac.ir/article-1-1630-en.html
URL: http://mlj.goums.ac.ir/article-1-1630-en.html
1- Department of Clinical Biochemistry University of Kashmir, Hazratbal, Srinagar, Kashmir, J&K India , ifrahreshi9@gmail.com
2- Department of Biochemistry Govt Medical College and associated hospitals, Karan Nagar, Srinagar, Kashmir, J&K India
2- Department of Biochemistry Govt Medical College and associated hospitals, Karan Nagar, Srinagar, Kashmir, J&K India
Full-Text [PDF 574 kb]
(1472 Downloads)
| Abstract (HTML) (6118 Views)
Full-Text: (1303 Views)
Introduction
In December 2019, a series of pneumonia cases of unknown cause emerged in Wuhan, Hubei, China, with clinical presentations greatly resembling viral pneumonia (1). WHO declared COVID-19 a global health emergency on January 30, 2020, and characterized it pandemic on 11 March 2020 (2). As there have been 775,335,916 confirmed cases of COVID-19, including 7,045,569 deaths worldwide reported to WHO, and India recorded a total of 45,035,393 COVID-19 cases, including 533,570 deaths. (3)
In inflammation seen in viral pneumonia, such as COVID-19, an imbalance of immune response is seen as a result of severe inflammatory response and poor immune response (4). As a result, circulating biomarkers of inflammation and the immune system can serve as reliable predictors of the prognosis for COVID-19 patients (5). Of these, white blood cell (WBC) count, neutrophil (NEU) to lymphocyte (LYM) ratio (NLR), and platelet to-lymphocyte-ratio (PLR) levels help predict the prognosis of patients with viral pneumonia. The neutrophil/lymphocyte ratio (NLR) is associated with the progression of the infection and can be utilized by physicians to identify high-risk or deteriorating patients at an early stage (6). NLR includes two different leukocyte subsets, reflecting both the degree of systemic inflammation and the equilibrium of the body's neutrophil and lymphocyte counts. It more properly depicts the balance between the degree of inflammation and the state of the body's immunity (7). The dNLR was derived from the assumption that the white cell count is made up primarily of lymphocytes and neutrophils, and therefore, the white cell count minus the neutrophil count would be broadly similar to the lymphocyte count (8). The platelet-to-lymphocyte-ratio (PLR) is an integrated reflection of two important opposite inflammatory pathways easily calculated from a complete blood count. Platelet to lymphocyte ratio is also an economical tool and more predictive than either the platelet or the lymphocyte counts alone. As markers of inflammation, various studies have demonstrated the correlation between NLR, d-NLR, PLR, and many diseases such as inflammatory diseases (9), cardiovascular diseases (10), cancer (11), and COVID-19 (12).
In this study, we comparatively analyzed the CBC profile and determined the association of the various CBC parameters with severity and disease outcome in SARS-CoV-2 infected patients from Kashmir with an ultimate aim to discover CBC parameters of diagnostic and/ prognostic significance in SARS-CoV-2 infected patients from Kashmir.
Methods
The study was performed on the patients admitted in the Government Medical College Srinagar and associated SMHS Hospital from Aug 2021 to Jan 2022. The purpose of the research was explained to the participants. All participants consented (in a written form) to be involved in this research. Patients who were COVID-19-positive (confirmed by RT-PCR of the swab) were included in the study. This observational Cohort study enrolled 75 Patients (48 females, 27 males). The patients were categorized based on the severity of the disease according to WHO guidelines (13): Moderately ill: Individuals who show evidence of lower respiratory disease during clinical assessment or imaging and who have an oxygen saturation measured by pulse oximetry (SpO2) ≥94% on room air at sea level. Severely ill: Individuals who have SpO2 <94% on room air at sea level, a ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) <300 mm Hg, a respiratory rate >30 breaths/min, or lung infiltrates >50% and, critically ill: Individuals who have respiratory failure, septic shock, and/or multiple organ dysfunction, which later failed to survive.
Inclusion criteria:
a) Patients group: 75 SARS-CoV-2 infected (confirmed by positive RT-PCR of the swab) patients admitted to the hospital for treating covid-19 of varying severity during the course of the study. The patients were followed until death or discharge for a maximum of 28 days.
b) Control group: 20 healthy individuals that were negative for SARS-CoV-2 confirmed by negative RT-PCR of the swab.
Exclusion criteria:
a) Immuno-compromised or patients with any immunological disorders.
Fully auto Sysmex-XN-1000 hematology analyzer was used for the analysis of the complete blood count.
The data was analyzed using IBM Statistical Package for the Social Sciences (SPSS) software 26. Descriptive statistics was performed and data was presented as frequency (N) and percentage (%). Continuous data was presented as mean and standard deviation. Chi-square test and student’s t test were used to compare proportions between groups as deemed proper by the statistical expert. ROC analysis was carried to determine the prognostic value of CBC parameters. A P- value of less than 0.05 was considered statistically significant.
Results
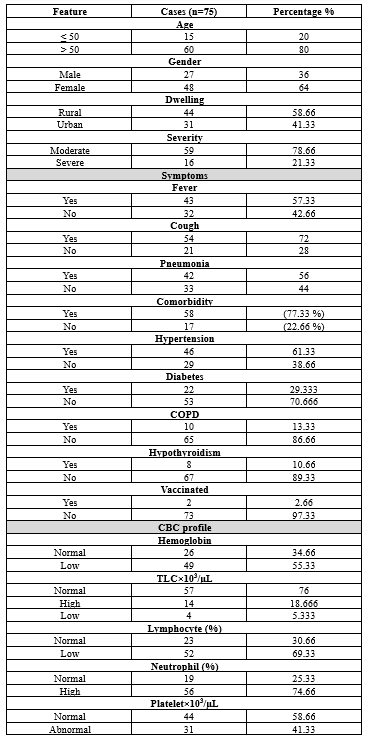
In this study, a total of 75 cases that were diagnosed (confirmed positive by RT-PCR) with COVID-19 and admitted to SMHS hospital for management were taken. The Socio-demographic and clinical characteristics of the cases are shown in Table 1. Out of total 75 patients, 78.66% of the cases were >50 years and were mostly females (64%) and most of the patients were of rural origin (58.66%). Among the patients under study, cough was the major symptom present (72% of cases) followed by fever (57.33%) and pneumonia (56%). Most of the CoV-2 infected patients admitted to our hospital were with comorbidities (77.33%) including hypertension (61.33%), diabetes (29.33%), COPD (13.33%), and hypothyroidism (10.66%). Based on the severity of the infection of SARS CoV-2 the patients were divided into two groups: moderate and severe (including critical). It was found that moderate cases were more (78.66%) than severe cases (21.33%). On comparative CBC analysis of COVID-19 patients (55.33%), it was found that the majority of the patients were having low levels of Hemoglobin. Among SARS-CoV-2 infected patients 69.33% were with low percentage of lymphocytes compared to normal. It was found that a greater % of covid-19 patients (74.66%) had high levels of neutrophils. It was observed that the platelet count was normal only in 58.666% of patients.
Table 2 represents comparison of CBC parameters (laboratory and derived values) of COVID-19 patients vs. non-infected. The significance of CBC parameters between COVID-19–positive and COVID-19–negative individuals was assessed by Student t test. Compared to normal individuals, mean Hemoglobin levels (13.43 Vs 10.9g/dl) (p=0.0001) (Figure 1a), Lymphocyte% (16.04 Vs 30.80) (Figure 1c), Monocyte% (5.53 Vs 7.53) (p=0.009) (Figure 1d), platelet count (150 Vs 186) (p=0.037) (Figure 1e) were significantly lower in SARS-COV-2 infected patients. Neutrophil % (76.77 Vs 59.26) (P=0.00001) was significantly higher (Figure 1b). Neutrophil-to-lymphocyte ratio (NLR) was significantly higher in covid-19 patients (7.31 Vs 2.04) (P=0.001) (Figure 1f), derived Neutrophil-to lymphocyte (dNLR) ratio was also significantly high (4.43 Vs 1.5) with p=0.0002 (Figure 1g).
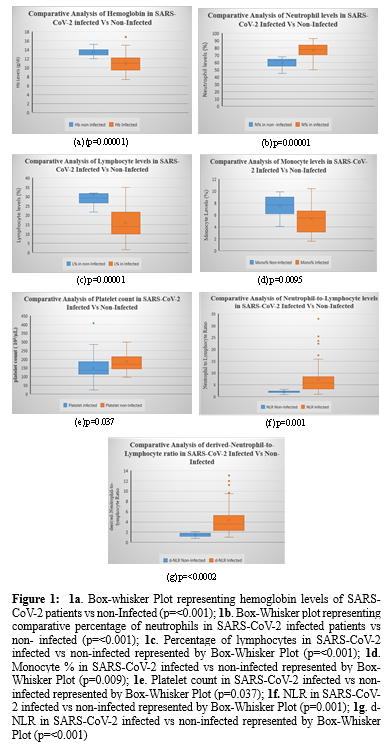
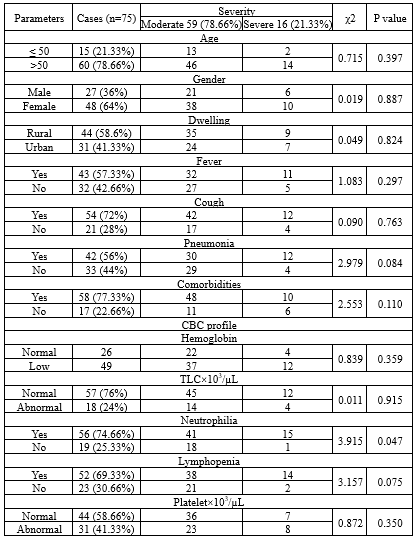
Table 3 represents association of socio-demographic features and clinical characteristics of SARS-CoV-2 Infected patients with the severity of disease. Significant association was found between high neutrophil percentage and the severity of the disease (p=0.047). Though not statistically significant an association was found between lymphopenia and severity of the COVID-19.
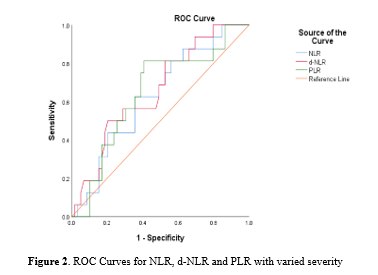
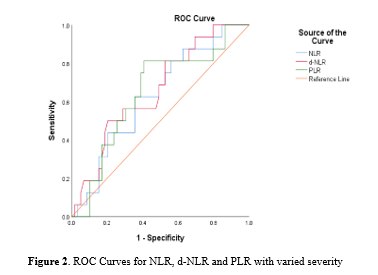
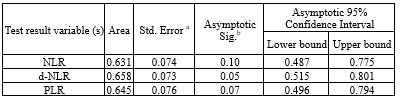
No defined laboratory reference values were found for NLR, d-NLR, PLR in SARS-CoV 2 infected patients. In order to find the association of NLR, d-NLR, PLR with severity of disease, we analyzed the optimal cut-off values for each of these parameters calculated by the ROC analysis, and the ROC curves were presented in Figure 2. The areas under the curve (AUC) of NLR, d-NLR, and PLR were 0.631, 0.658, and 0.645 respectively (Table 4). Though each of these parameters revealed an association with the severity of the disease, however, AUC of d-NLR was found statistically significant (p=0.05). The optimal cut-off value for d-NLR was 3.45 with sensitivity (68%) and specificity (50%).
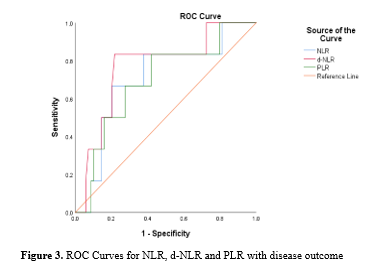
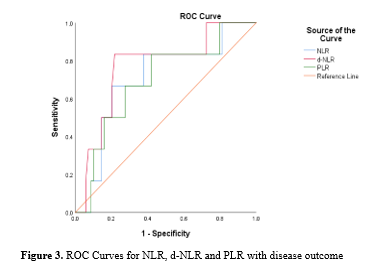
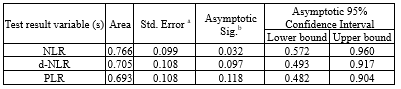
The ROC curves, using COVID-19 Specific death as an end-point for NLR, dNLR and PLR is shown in Figure 3. The areas under the curve (AUC) of d-NLR, NLR, and PLR were 0.766, 0.705, and 0.693 respectively (Table 5). Out of these, only d-NLR was found statistically significant (p=0.03). The optimal cut-off value of d-NLR for predicting disease outcome was 5.1. The highest sensitivity and specificity were 83% and 78% respectively.
Discussion
Severe acute respiratory syndrome coronavirus (SARS-COV-2), known as COVID-19, is the new type of coronavirus responsible for the latest pandemic in the world (14). There are different clinical characteristics and laboratory findings that has been associated with severity, hospitalization, and mortality in COVID-19 (15). Among the baseline investigations, CBC analysis has an important role in the monitoring and management of COVID-19. Therefore, the present study aimed to comparatively analyze CBC parameters (normal and derived) in SARS-CoV-2 infected patients and normal non- infected subjects admitted to SMHS hospital from Kashmir. In the present study hemoglobin, neutrophils, lymphocytes, monocytes were found the most common deranged CBC parameters in SARS-CoV-2 infected patients. Analysis of derived CBC parameters revealed dNLR as an early predictive marker of disease severity and poor disease outcome in SARS-CoV-2 patients from Kashmir. On CBC analyses of peripheral blood, Hemoglobin was found significantly low in COVID-19 patients. The possible mechanism of low Hb in SARS-CoV-2 infected patients could be the inflammation that can alter iron hemostasis and reduce intestinal iron absorption, resulting in the reduced availability of the metal for erythropoiesis and the production of hemoglobin (Hb) (16). In our study Neutrophil count was found significantly high among the SARS-CoV-2 Infected patients compared to normal (p=0.0001). Neutrophil is a major component of the leukocyte population that activates and migrates from the venous system to the immune organ or system upon infection. Moreover, neutrophil can also be activated by virus-related inflammatory factors, such as IL-6 and IL-8, TNF-α and G-CSF, and INF-γ factors, produced by lymphocyte and endothelial cells (17-20). Neutrophils are known to release large amounts of ROS that can induce cell damage and free the virus from the cells. The antibody dependent cell mediated cell (ADCC) may kill the virus directly or expose virus antigen and stimulate cell-specific and humoral immune response (21). In addition, neutrophils are reported to increase the expression of 45 circulating vascular endothelial growth factor (VEGF) in COVID-19 patients (22) that markedly contributes to tissue and organ damage. This fact was substantiated here also as the significant association was found between high neutrophil percentage and the severity of disease (Table 4). Lymphopenia is a common feature in COVID-19 so was found in this study. Lymphocytes play a conclusive role in upholding immune homeostasis and inflammatory response throughout the body. On comparative analysis, lymphocytes were significantly low in SARS-CoV-2 infected patients (p=0.0001). There are four possible potential mechanisms that can lead to lymphocyte deficiency in SARS-CoV-2 infected patients. (i) The SARS-CoV-2 virus might directly infect lymphocytes as they bear ACE2 receptors which are its common targets (23). (ii) The SARS-CoV-2 virus might directly destroy lymphatic organs such as thymus and spleen decreasing the production of lymphocytes. (iii) Inflammatory cytokines like tumor necrosis factor (TNF)α, interleukin (IL)-6, have been found deranged in SARS-CoV-2 infected patients perhaps leading to lymphocyte apoptosis (24). (iv) Inhibition of lymphocytes by metabolic molecules produced by metabolic disorders, such as hyperlactic acidemia as reported in the severe type of COVID-19 patients (25). Decreased monocyte cells are also a characteristic feature of COVID-19 so was observed in our study. On comparative analysis the monocytosis was found significantly low among SARS-CoV-2 infected patients (p=0.009). Acute and chronic inflammation results in systemic monocytosis so is observed in SARS infected patients. Monocytes are recruited to inflammatory sites where they mediate inflammation and differentiate into tissue macrophages. Blood monocytosis enables eradication of infection and removal of cellular debris after injury and ischemia. Monocyte-derived macrophages may also support resolution of inflammation, if their phenotype permits. However, exaggerated monocytosis during inflammation likely harms tissues by limiting resolution of inflammation and propagating exaggerated immune activation (26). On comparative analysis significantly low levels of platelet count was found in SARS infected patients compared to normal individual (p=0.03). So reduced platelet count is characteristic CBC feature associated with COVID-19 infection. The low platelet count, generally observed in viral infections can lead to thrombocytopenia in SARS-CoV-2 infected patients too. The possible reason for low platelet count is the activation of platelets either by viral antigen antibody complexes or host inflammatory responses leading to clearance of activated platelets by the reticuloendothelial system (27). Viruses can also interact with megakaryocytes and reduce platelet synthesis so must be true for SARS-CoV-2. (28). After the discussion of the basic parameters of Complete Blood Count of COVID-19, we analyzed the different ratios of CBC parameters which include NLR, PLR, d-NLR in patients with COVID-19. From the AUC analysis of NLR, dNLR and PLR, d-NLR was found as an early prognostic biomarker of disease severity in SARS-CoV-2 infected patients. The applicable thresholds for NLR, d-NLR, PLR, were observed using the ROC curve. The optimal threshold at 3.45 for d-NLR showed a superior prognostic risk of clinical symptoms to change from mild to severe, which had the highest of sensitivity (68%) and specificity (50%) and the largest of AUC i.e., 0.658. So, these patients require diligent attention by clinician. On ROC curve analysis of derived parameters d-NLR was the only significant parameter to predict poor disease outcome with AUC= 0.766 having highest specificity (78%) and sensitivity (83%).
Conclusion
From this study, we concluded among CBC parameters increased neutrophilia as significantly associated with the severity of disease. Among the derived CBC parameters, d- NLR, turns out to be a predictive biomarker for severity of the disease (AUC=0.658, at specificity of 50% and sensitivity of 68%) as well as for poor disease outcome (AUC=0.766, at specificity of 78% and sensitivity of 83%).
Acknowledgement
Multi-disciplinary Research Unit (MRU), GMC Srinagar. Department of Pathology, GMC Srinagar.
Funding sources
Not applicable
Ethical statement
The work was ethically approved by the ethical committee of GOVT Medical College and associated SMHS Hospital. Approval no: Ref No.IEC-GMC-Sgr/27.
Conflicts of interest
The authors declare no conflict of interest.
Author contributions
Authors IJ and RE have contributed to the design and implementation of the study. Authors IJ and IF have carried out the data collection of the work. Authors IJ and IF did the formal analysis. Author SF investigated the work. Authors IJ, SS, RE, and SM wrote the original draft as well as edited the manuscript. The final manuscript was read and approved by all authors.
In December 2019, a series of pneumonia cases of unknown cause emerged in Wuhan, Hubei, China, with clinical presentations greatly resembling viral pneumonia (1). WHO declared COVID-19 a global health emergency on January 30, 2020, and characterized it pandemic on 11 March 2020 (2). As there have been 775,335,916 confirmed cases of COVID-19, including 7,045,569 deaths worldwide reported to WHO, and India recorded a total of 45,035,393 COVID-19 cases, including 533,570 deaths. (3)
In inflammation seen in viral pneumonia, such as COVID-19, an imbalance of immune response is seen as a result of severe inflammatory response and poor immune response (4). As a result, circulating biomarkers of inflammation and the immune system can serve as reliable predictors of the prognosis for COVID-19 patients (5). Of these, white blood cell (WBC) count, neutrophil (NEU) to lymphocyte (LYM) ratio (NLR), and platelet to-lymphocyte-ratio (PLR) levels help predict the prognosis of patients with viral pneumonia. The neutrophil/lymphocyte ratio (NLR) is associated with the progression of the infection and can be utilized by physicians to identify high-risk or deteriorating patients at an early stage (6). NLR includes two different leukocyte subsets, reflecting both the degree of systemic inflammation and the equilibrium of the body's neutrophil and lymphocyte counts. It more properly depicts the balance between the degree of inflammation and the state of the body's immunity (7). The dNLR was derived from the assumption that the white cell count is made up primarily of lymphocytes and neutrophils, and therefore, the white cell count minus the neutrophil count would be broadly similar to the lymphocyte count (8). The platelet-to-lymphocyte-ratio (PLR) is an integrated reflection of two important opposite inflammatory pathways easily calculated from a complete blood count. Platelet to lymphocyte ratio is also an economical tool and more predictive than either the platelet or the lymphocyte counts alone. As markers of inflammation, various studies have demonstrated the correlation between NLR, d-NLR, PLR, and many diseases such as inflammatory diseases (9), cardiovascular diseases (10), cancer (11), and COVID-19 (12).
In this study, we comparatively analyzed the CBC profile and determined the association of the various CBC parameters with severity and disease outcome in SARS-CoV-2 infected patients from Kashmir with an ultimate aim to discover CBC parameters of diagnostic and/ prognostic significance in SARS-CoV-2 infected patients from Kashmir.
Methods
The study was performed on the patients admitted in the Government Medical College Srinagar and associated SMHS Hospital from Aug 2021 to Jan 2022. The purpose of the research was explained to the participants. All participants consented (in a written form) to be involved in this research. Patients who were COVID-19-positive (confirmed by RT-PCR of the swab) were included in the study. This observational Cohort study enrolled 75 Patients (48 females, 27 males). The patients were categorized based on the severity of the disease according to WHO guidelines (13): Moderately ill: Individuals who show evidence of lower respiratory disease during clinical assessment or imaging and who have an oxygen saturation measured by pulse oximetry (SpO2) ≥94% on room air at sea level. Severely ill: Individuals who have SpO2 <94% on room air at sea level, a ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) <300 mm Hg, a respiratory rate >30 breaths/min, or lung infiltrates >50% and, critically ill: Individuals who have respiratory failure, septic shock, and/or multiple organ dysfunction, which later failed to survive.
Inclusion criteria:
a) Patients group: 75 SARS-CoV-2 infected (confirmed by positive RT-PCR of the swab) patients admitted to the hospital for treating covid-19 of varying severity during the course of the study. The patients were followed until death or discharge for a maximum of 28 days.
b) Control group: 20 healthy individuals that were negative for SARS-CoV-2 confirmed by negative RT-PCR of the swab.
Exclusion criteria:
a) Immuno-compromised or patients with any immunological disorders.
Fully auto Sysmex-XN-1000 hematology analyzer was used for the analysis of the complete blood count.
The data was analyzed using IBM Statistical Package for the Social Sciences (SPSS) software 26. Descriptive statistics was performed and data was presented as frequency (N) and percentage (%). Continuous data was presented as mean and standard deviation. Chi-square test and student’s t test were used to compare proportions between groups as deemed proper by the statistical expert. ROC analysis was carried to determine the prognostic value of CBC parameters. A P- value of less than 0.05 was considered statistically significant.
Results
In this study, a total of 75 cases that were diagnosed (confirmed positive by RT-PCR) with COVID-19 and admitted to SMHS hospital for management were taken. The Socio-demographic and clinical characteristics of the cases are shown in Table 1. Out of total 75 patients, 78.66% of the cases were >50 years and were mostly females (64%) and most of the patients were of rural origin (58.66%). Among the patients under study, cough was the major symptom present (72% of cases) followed by fever (57.33%) and pneumonia (56%). Most of the CoV-2 infected patients admitted to our hospital were with comorbidities (77.33%) including hypertension (61.33%), diabetes (29.33%), COPD (13.33%), and hypothyroidism (10.66%). Based on the severity of the infection of SARS CoV-2 the patients were divided into two groups: moderate and severe (including critical). It was found that moderate cases were more (78.66%) than severe cases (21.33%). On comparative CBC analysis of COVID-19 patients (55.33%), it was found that the majority of the patients were having low levels of Hemoglobin. Among SARS-CoV-2 infected patients 69.33% were with low percentage of lymphocytes compared to normal. It was found that a greater % of covid-19 patients (74.66%) had high levels of neutrophils. It was observed that the platelet count was normal only in 58.666% of patients.
|
Table1. Socio-Demographic and clinical features of RT-PCR confirmed SARS-COV-2 infected patients admitted to SMHS Hospital (N=75)
 |
|
Table 2. Comparative analysis of CBC profile of SARS-COV-2 infected vs non- infected (Controls)
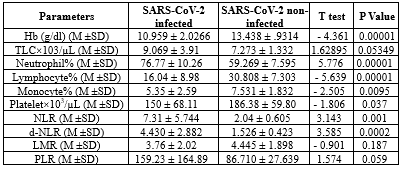 |
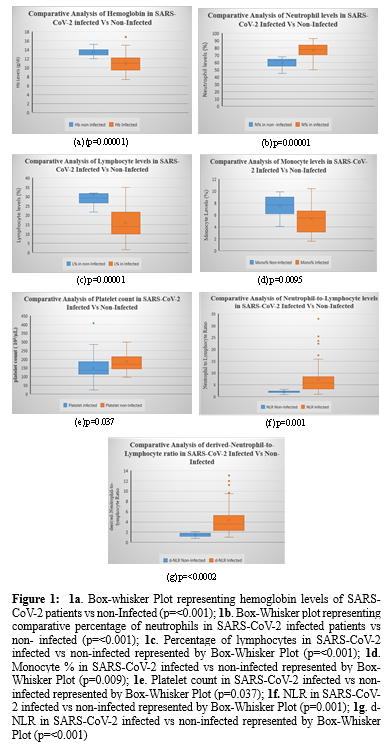
Table 3 represents association of socio-demographic features and clinical characteristics of SARS-CoV-2 Infected patients with the severity of disease. Significant association was found between high neutrophil percentage and the severity of the disease (p=0.047). Though not statistically significant an association was found between lymphopenia and severity of the COVID-19.
|
Table 3. Association of various socio-demographic features and CBC parameters of SARS-CoV-2 patients with the severity of disease
 |
|
Table 4. Areas under curve (AUC) for NLR, d-NLR, and PLR for severity
 |
|
Table 5. Areas under curve (AUC) for d-NLR, NLR, and PLR for disease outcome
 |
Discussion
Severe acute respiratory syndrome coronavirus (SARS-COV-2), known as COVID-19, is the new type of coronavirus responsible for the latest pandemic in the world (14). There are different clinical characteristics and laboratory findings that has been associated with severity, hospitalization, and mortality in COVID-19 (15). Among the baseline investigations, CBC analysis has an important role in the monitoring and management of COVID-19. Therefore, the present study aimed to comparatively analyze CBC parameters (normal and derived) in SARS-CoV-2 infected patients and normal non- infected subjects admitted to SMHS hospital from Kashmir. In the present study hemoglobin, neutrophils, lymphocytes, monocytes were found the most common deranged CBC parameters in SARS-CoV-2 infected patients. Analysis of derived CBC parameters revealed dNLR as an early predictive marker of disease severity and poor disease outcome in SARS-CoV-2 patients from Kashmir. On CBC analyses of peripheral blood, Hemoglobin was found significantly low in COVID-19 patients. The possible mechanism of low Hb in SARS-CoV-2 infected patients could be the inflammation that can alter iron hemostasis and reduce intestinal iron absorption, resulting in the reduced availability of the metal for erythropoiesis and the production of hemoglobin (Hb) (16). In our study Neutrophil count was found significantly high among the SARS-CoV-2 Infected patients compared to normal (p=0.0001). Neutrophil is a major component of the leukocyte population that activates and migrates from the venous system to the immune organ or system upon infection. Moreover, neutrophil can also be activated by virus-related inflammatory factors, such as IL-6 and IL-8, TNF-α and G-CSF, and INF-γ factors, produced by lymphocyte and endothelial cells (17-20). Neutrophils are known to release large amounts of ROS that can induce cell damage and free the virus from the cells. The antibody dependent cell mediated cell (ADCC) may kill the virus directly or expose virus antigen and stimulate cell-specific and humoral immune response (21). In addition, neutrophils are reported to increase the expression of 45 circulating vascular endothelial growth factor (VEGF) in COVID-19 patients (22) that markedly contributes to tissue and organ damage. This fact was substantiated here also as the significant association was found between high neutrophil percentage and the severity of disease (Table 4). Lymphopenia is a common feature in COVID-19 so was found in this study. Lymphocytes play a conclusive role in upholding immune homeostasis and inflammatory response throughout the body. On comparative analysis, lymphocytes were significantly low in SARS-CoV-2 infected patients (p=0.0001). There are four possible potential mechanisms that can lead to lymphocyte deficiency in SARS-CoV-2 infected patients. (i) The SARS-CoV-2 virus might directly infect lymphocytes as they bear ACE2 receptors which are its common targets (23). (ii) The SARS-CoV-2 virus might directly destroy lymphatic organs such as thymus and spleen decreasing the production of lymphocytes. (iii) Inflammatory cytokines like tumor necrosis factor (TNF)α, interleukin (IL)-6, have been found deranged in SARS-CoV-2 infected patients perhaps leading to lymphocyte apoptosis (24). (iv) Inhibition of lymphocytes by metabolic molecules produced by metabolic disorders, such as hyperlactic acidemia as reported in the severe type of COVID-19 patients (25). Decreased monocyte cells are also a characteristic feature of COVID-19 so was observed in our study. On comparative analysis the monocytosis was found significantly low among SARS-CoV-2 infected patients (p=0.009). Acute and chronic inflammation results in systemic monocytosis so is observed in SARS infected patients. Monocytes are recruited to inflammatory sites where they mediate inflammation and differentiate into tissue macrophages. Blood monocytosis enables eradication of infection and removal of cellular debris after injury and ischemia. Monocyte-derived macrophages may also support resolution of inflammation, if their phenotype permits. However, exaggerated monocytosis during inflammation likely harms tissues by limiting resolution of inflammation and propagating exaggerated immune activation (26). On comparative analysis significantly low levels of platelet count was found in SARS infected patients compared to normal individual (p=0.03). So reduced platelet count is characteristic CBC feature associated with COVID-19 infection. The low platelet count, generally observed in viral infections can lead to thrombocytopenia in SARS-CoV-2 infected patients too. The possible reason for low platelet count is the activation of platelets either by viral antigen antibody complexes or host inflammatory responses leading to clearance of activated platelets by the reticuloendothelial system (27). Viruses can also interact with megakaryocytes and reduce platelet synthesis so must be true for SARS-CoV-2. (28). After the discussion of the basic parameters of Complete Blood Count of COVID-19, we analyzed the different ratios of CBC parameters which include NLR, PLR, d-NLR in patients with COVID-19. From the AUC analysis of NLR, dNLR and PLR, d-NLR was found as an early prognostic biomarker of disease severity in SARS-CoV-2 infected patients. The applicable thresholds for NLR, d-NLR, PLR, were observed using the ROC curve. The optimal threshold at 3.45 for d-NLR showed a superior prognostic risk of clinical symptoms to change from mild to severe, which had the highest of sensitivity (68%) and specificity (50%) and the largest of AUC i.e., 0.658. So, these patients require diligent attention by clinician. On ROC curve analysis of derived parameters d-NLR was the only significant parameter to predict poor disease outcome with AUC= 0.766 having highest specificity (78%) and sensitivity (83%).
Conclusion
From this study, we concluded among CBC parameters increased neutrophilia as significantly associated with the severity of disease. Among the derived CBC parameters, d- NLR, turns out to be a predictive biomarker for severity of the disease (AUC=0.658, at specificity of 50% and sensitivity of 68%) as well as for poor disease outcome (AUC=0.766, at specificity of 78% and sensitivity of 83%).
Acknowledgement
Multi-disciplinary Research Unit (MRU), GMC Srinagar. Department of Pathology, GMC Srinagar.
Funding sources
Not applicable
Ethical statement
The work was ethically approved by the ethical committee of GOVT Medical College and associated SMHS Hospital. Approval no: Ref No.IEC-GMC-Sgr/27.
Conflicts of interest
The authors declare no conflict of interest.
Author contributions
Authors IJ and RE have contributed to the design and implementation of the study. Authors IJ and IF have carried out the data collection of the work. Authors IJ and IF did the formal analysis. Author SF investigated the work. Authors IJ, SS, RE, and SM wrote the original draft as well as edited the manuscript. The final manuscript was read and approved by all authors.
Research Article: Research Article |
Subject:
Biochemistry
Received: 2023/02/20 | Accepted: 2023/12/13 | Published: 2024/01/21 | ePublished: 2024/01/21
Received: 2023/02/20 | Accepted: 2023/12/13 | Published: 2024/01/21 | ePublished: 2024/01/21
References
1. WHO. Novel coronavirus - China. 2020. [View at Publisher] [Google Scholar]
2. WHO. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. [View at Publisher]
3. WHO. WHO COVID-19 dashboard: COVID-19 cases. 2023. [View at Publisher]
4. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727-33. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Xiang N, Havers F, Chen T, Song Y, Tu W, Li L, et al. Use of national pneumonia surveillance to describe influenza A (H7N9) virüs epidemiology, China, 2004-2013. Emerg Infect Dis. 2013;19(11):1784‐90. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Feng X, Li S, Sun Q, Zhu J, Chen B, Xiong M, et al. Immune-Inflammatory Parameters in COVID-19 Cases: A Systematic Review and Meta-Analysis. Front Med. 2020;7:301. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Soylu K, Gedikli Ö, Ekşi A, Avcıoğlu Y, İdil Soylu A, Yüksel S et al. Neutrophil-to-lymphocyte ratio for the assessment of hospital mortality in patients with acute pulmonary embolism. Arch Med Sci. 2016;12(1):95-100. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Proctor MJ, McMillan DC, Morrison DS, Fletcher CD, Horgan PG, Clarke SJ. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br J Cancer. 2012;107:695-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Alan S, Tuna S, Türkoğlu EB. The relation of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume with the presence and severity of Behçet's syndrome. Kaohsiung J Med Sci. 2015;31(12):626-31. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Wang X, Zhang G, Jiang X, Zhu H, Lu Z, Xu L. Neutrophil to lymphocyte ratio in relation to risk of all-cause mortality and cardiovascular events among patients undergoing angiography or cardiac revascularization: a meta-analysis of observational studies. Atherosclerosis. 2014;234(1):206-13. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Bowen RC, Little NAB, Harmer JR, Ma J, Mirabelli LG, Roller KD, et al. Neutrophil-to-lymphocyte ratio as prognostic indicator in gastrointestinal cancers: a systematic review and meta-analysis. Oncotarget. 2017;8(19):32171-89 [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d‐NLR and PLR in COVID‐19 patients. Int Immunopharmacol. 2020;84:106504. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. National Institutes of Health. COVID-19 Treatment Guidelines Panel; Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. 2022. [View at Publisher]
14. Raoult D, Zumla A, Locatelli F, Ippolito G, Kroemer G. Coronavirus infections: epidemiological, clinical and immunological features and hypotheses. Cell Stress. 2020;4(4):66-75. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Cecconi M, Piovani D, Brunetta E, Aghemo A, Greco M, Ciccarelli M, et al. Early predictors of clinical deterioration in a cohort of 239 patients hospitalized for Covid-19 infection in Lombardy, Italy. J Clin Med. 2020;9(5):1548. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Bellmann-Weiler R, Lanser L, Barket R, Rangger L, Schapfl A, Schaber M, et al. Prevalence and predictive value of Anemia and Dysregulated Iron homeostasis in patients with COVID-19 infection. J Clin Med. 2020;9(8):2429. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Kuper H, Adami HO, Trichopoulos D. Infections as a major preventable cause of human cancer. J Intern Med. 2000;248(3):171-183. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Blaser MJ, Chyou PH, Nomura A. Age at Establishment of Helicobacter pylori Infection and Gastric Carcinoma, Gastric Ulcer, and Duodenal Ulcer Risk. Cancer Res. 1995;55(3):562-5. [View at Publisher] [PMID] [Google Scholar]
19. Scholl SM, Pallud C, Beuvon F, Hacene K, Stanley ER, Rohrschneider L, et al. Anti-colony-stimulating factor-1 antibody staining in primary breast adenocarcinomas correlates with marked inflammatory cell infiltrates and prognosis. J NatI Cancer Inst. 1994;86(2):120-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Shacter E, Weitzman SA. Chronic inflammation and cancer. Oncology (Williston Park). 2002;16(2):217-26. [View at Publisher] [PMID] [Google Scholar]
21. Kusumanto YH, Dam WA, Hospers GAP, Meijer C, Mulder NH. Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis. 2003;6(4):283-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Kim SL, Lee ST, Trang KTT, Kim SH, Kim IH, Lee SO. Parthenolide exerts inhibitory effects on angiogenesis through the downregulation of VEGF/VEGFRs in colorectal cancer. Int J Mol Med. 2014;33(5):1261-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):8. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Liao YC, Liang WG, Chen FW, Hsu JH, Yang JJ, Chang MS. IL-19 induces production of IL-6 and TNF-alpha and results in cell apoptosis through TNF-alpha. J Immunol. 2002;169(8):4288-97. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Fischer K, Hoffmann P, Voelkl S, Meidenbauer N, Ammer J, Edinger M, et al. Inhibitory effect of tumor cell-derived lactic acid on human T cells. Blood. 2007;109(9):3812-19. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Dutta P, Nahrendorf M. Regulation and consequences of monocytosis. Immunol Rev. 2014;262(1):167-78. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Assinger A. Platelets and infection - an emerging role of platelets in viral infection. Front Immunol. 2014;5:649. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Seyoum M, Enawgaw B, Melku M. Human blood platelets and viruses: defense mechanism and role in the removal of viral pathogens. Thromb J. 2018;16(1):16. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








 goums.ac.ir
goums.ac.ir yahoo.com
yahoo.com