Volume 18, Issue 1 (Jan-Feb 2024)
mljgoums 2024, 18(1): 32-33 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
. S, Jamal I, Choudhary V. Primary plasma cell leukemia in a 19-Year-Old female: An unusual presentation of a rare entity. mljgoums 2024; 18 (1) :32-33
URL: http://mlj.goums.ac.ir/article-1-1604-en.html
URL: http://mlj.goums.ac.ir/article-1-1604-en.html
1- Department of Hematology, Igims Patna, India
2- Department of Hematology, Igims Patna, India ,iffatjamal111@gmail.com
2- Department of Hematology, Igims Patna, India ,
Full-Text [PDF 367 kb]
(1154 Downloads)
| Abstract (HTML) (5450 Views)
Full-Text: (1316 Views)
Introduction
Plasma cell leukemia (PCL) is a rare yet aggressive malignancy, comprising 1-2% of all plasma cell dyscrasias (1). It can manifest either as a de novo condition (primary) or as a result of leukemic transformation in advanced multiple myeloma (MM). Plasma cell leukemia is clinically and biologically different from MM, typically diagnosed at a younger age, displaying a greater tendency for visceral and extramedullary involvement and presenting unique biologic, immunophenotypic, and cytogenetic characteristics. As a result, its accurate and timely diagnosis is crucial for appropriate management (2).
Case report
A 19-year-old female presented to the Hematology Department of the Indira Gandhi Institute of Medical Sciences in Patna, India, in May 2022, with a 1-month history of fever, headache, and weakness. Her medical and family history was unremarkable. During the clinical examination, the only notable finding was unexplained pallor that did not respond to hematinics. Her hemogram revealed the following: a hemoglobin level of 5.0 g/dL, a total white blood cell count of 14.9 x 109/L, and a platelet count of 149 x 109/L. The peripheral smear showed a microcytic hypochromic picture with Rouleaux formation, along with the presence of 36% plasma cells, including plasmacytoid lymphocytes (Figure 1a).

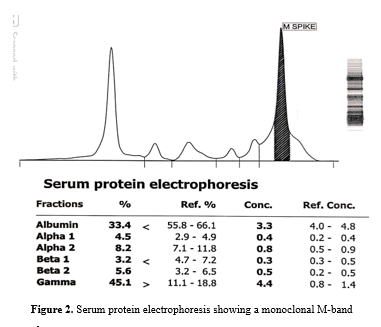
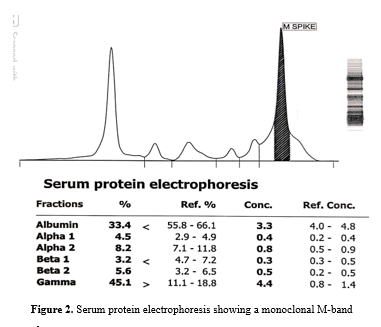
Bone marrow aspiration smears were hemodiluted and showed infiltration by approximately 50% plasma cells, including abnormal forms. Many plasma cells were observed in clusters entangled in a fibrin meshwork (Figure 1b). The bone marrow biopsy was hypercellular, with findings consistent with plasma cell dyscrasia (Figure 1c). An ultrasound scan of the abdomen revealed no organomegaly or lymphadenopathy. Liver and renal function tests showed hypoalbuminemia, hyperphosphatemia, hyperuricemia, and elevated creatinine levels (5.2 mg/dL). Serum protein electrophoresis (SPE) and immunofixation studies indicated the presence of immunoglobulin G (IgG) kappa paraprotein at a concentration of 4.3 g/dL. A skeletal survey showed no osteolytic lesions.
Immunohistochemistry performed on the bone marrow biopsy showed positivity for CD38 and CD138 with kappa light chain restriction, while lambda light chain was negative (Figures 1b to 1f). Serum protein electrophoresis revealed a monoclonal M band (Figure 2).
Unfortunately, the patient succumbed to her illness before the initiation of treatment.
Discussion
Plasma cell leukemia is a highly aggressive neoplasm with no consensus on a standard chemotherapy regimen due to its rarity. It comprises fewer than 1 patient per 1 000 000 population (3). It is characterized by the presence of >20% plasma cells in peripheral blood, with its incidence ranging from 2% to 4% of all myelomas (4,5). It has 2 variants - the primary form, which arises de novo in patients with no previous history of multiple myeloma, constituting 60%, and the secondary form, which consists of a leukemic transformation in previously recognized multiple myeloma, constituting the remaining 40% of total cases (6).
Phenotypically, these cells originate from the proliferation of CD38-expressing plasma cells. A minority of cells also express CD10, HLA-DR, and CD20. Primary PCL shows higher expression of CD20 compared to multiple myeloma (7). Additionally, plasma cells from both primary and secondary PCL lack CD56, which is important for anchoring plasma cells to bone marrow stroma. More than 80% have a diploid/hypodiploid DNA content, (6,8) and cytogenetic studies show complex karyotypes with multiple numerical and structural abnormalities. Up to 90% may show chromosome 13 monosomy (8).
Due to the low frequency of PCL, most of the data has come from case reports or small series of cases. In almost all the series, the median age ranged between 53 and 57 years (about 10 years younger than the median age in the myeloma series). The youngest age reported was 30 years (6).
Primary PCL follows a more aggressive course with a higher frequency of extramedullary involvement in the liver, spleen, and lymph nodes. It is also clinically more severe, manifesting as thrombocytopenia, anemia, hypercalcemia, and impaired renal function. Garcia-Sanz et al. identified ten variables with unfavorable prognostic value on the survival of primary PCL cases, of which a serum beta 2 microglobulin level > 6mg/L and S-phase bone marrow plasma cells >4.5% retained independent value on multivariate analysis (9).
Response to treatment for PCL is poor, with a median survival of less than 1 year, and the longest survival reported was 28 months (5). Failing to achieve 50% clearance of blood plasma cells within 10 days after the initiation of treatment is a predictor of no response (3,8).
Using a single alkylating agent with prednisolone is not appropriate for patients with primary PCL. Survival is significantly better in PCL patients treated with polychemotherapy compared to melphalan and prednisolone (9). Drugs used include vincristine, adriamycin, dexamethasone, and/or cyclophosphamide and etoposide (8). Alternatively, VCMP/VBAP is also used.
Since the prognosis is so poor, intensification of high-dose chemotherapy followed by allogeneic/autologous stem cell rescue should be considered (8,9).
Conclusion
This case report emphasizes its rarity, young age at presentation, and the unusual clinical and laboratory findings. Persistent anemia unresponsive to standard treatment should raise the index of suspicion and prompt further investigations aimed at excluding uncommon malignancies.
Ethical statement
Ethical clearance was obtained from the Institutional Ethical Committee with reference number (318/IEC/IGIMS/2022).
Conflicts of interest
None
Patient consent
Written informed consent was duly obtained.
Plasma cell leukemia (PCL) is a rare yet aggressive malignancy, comprising 1-2% of all plasma cell dyscrasias (1). It can manifest either as a de novo condition (primary) or as a result of leukemic transformation in advanced multiple myeloma (MM). Plasma cell leukemia is clinically and biologically different from MM, typically diagnosed at a younger age, displaying a greater tendency for visceral and extramedullary involvement and presenting unique biologic, immunophenotypic, and cytogenetic characteristics. As a result, its accurate and timely diagnosis is crucial for appropriate management (2).
Case report
A 19-year-old female presented to the Hematology Department of the Indira Gandhi Institute of Medical Sciences in Patna, India, in May 2022, with a 1-month history of fever, headache, and weakness. Her medical and family history was unremarkable. During the clinical examination, the only notable finding was unexplained pallor that did not respond to hematinics. Her hemogram revealed the following: a hemoglobin level of 5.0 g/dL, a total white blood cell count of 14.9 x 109/L, and a platelet count of 149 x 109/L. The peripheral smear showed a microcytic hypochromic picture with Rouleaux formation, along with the presence of 36% plasma cells, including plasmacytoid lymphocytes (Figure 1a).

Bone marrow aspiration smears were hemodiluted and showed infiltration by approximately 50% plasma cells, including abnormal forms. Many plasma cells were observed in clusters entangled in a fibrin meshwork (Figure 1b). The bone marrow biopsy was hypercellular, with findings consistent with plasma cell dyscrasia (Figure 1c). An ultrasound scan of the abdomen revealed no organomegaly or lymphadenopathy. Liver and renal function tests showed hypoalbuminemia, hyperphosphatemia, hyperuricemia, and elevated creatinine levels (5.2 mg/dL). Serum protein electrophoresis (SPE) and immunofixation studies indicated the presence of immunoglobulin G (IgG) kappa paraprotein at a concentration of 4.3 g/dL. A skeletal survey showed no osteolytic lesions.
Immunohistochemistry performed on the bone marrow biopsy showed positivity for CD38 and CD138 with kappa light chain restriction, while lambda light chain was negative (Figures 1b to 1f). Serum protein electrophoresis revealed a monoclonal M band (Figure 2).
Unfortunately, the patient succumbed to her illness before the initiation of treatment.
Discussion
Plasma cell leukemia is a highly aggressive neoplasm with no consensus on a standard chemotherapy regimen due to its rarity. It comprises fewer than 1 patient per 1 000 000 population (3). It is characterized by the presence of >20% plasma cells in peripheral blood, with its incidence ranging from 2% to 4% of all myelomas (4,5). It has 2 variants - the primary form, which arises de novo in patients with no previous history of multiple myeloma, constituting 60%, and the secondary form, which consists of a leukemic transformation in previously recognized multiple myeloma, constituting the remaining 40% of total cases (6).
Phenotypically, these cells originate from the proliferation of CD38-expressing plasma cells. A minority of cells also express CD10, HLA-DR, and CD20. Primary PCL shows higher expression of CD20 compared to multiple myeloma (7). Additionally, plasma cells from both primary and secondary PCL lack CD56, which is important for anchoring plasma cells to bone marrow stroma. More than 80% have a diploid/hypodiploid DNA content, (6,8) and cytogenetic studies show complex karyotypes with multiple numerical and structural abnormalities. Up to 90% may show chromosome 13 monosomy (8).
Due to the low frequency of PCL, most of the data has come from case reports or small series of cases. In almost all the series, the median age ranged between 53 and 57 years (about 10 years younger than the median age in the myeloma series). The youngest age reported was 30 years (6).
Primary PCL follows a more aggressive course with a higher frequency of extramedullary involvement in the liver, spleen, and lymph nodes. It is also clinically more severe, manifesting as thrombocytopenia, anemia, hypercalcemia, and impaired renal function. Garcia-Sanz et al. identified ten variables with unfavorable prognostic value on the survival of primary PCL cases, of which a serum beta 2 microglobulin level > 6mg/L and S-phase bone marrow plasma cells >4.5% retained independent value on multivariate analysis (9).
Response to treatment for PCL is poor, with a median survival of less than 1 year, and the longest survival reported was 28 months (5). Failing to achieve 50% clearance of blood plasma cells within 10 days after the initiation of treatment is a predictor of no response (3,8).
Using a single alkylating agent with prednisolone is not appropriate for patients with primary PCL. Survival is significantly better in PCL patients treated with polychemotherapy compared to melphalan and prednisolone (9). Drugs used include vincristine, adriamycin, dexamethasone, and/or cyclophosphamide and etoposide (8). Alternatively, VCMP/VBAP is also used.
Since the prognosis is so poor, intensification of high-dose chemotherapy followed by allogeneic/autologous stem cell rescue should be considered (8,9).
Conclusion
This case report emphasizes its rarity, young age at presentation, and the unusual clinical and laboratory findings. Persistent anemia unresponsive to standard treatment should raise the index of suspicion and prompt further investigations aimed at excluding uncommon malignancies.
Ethical statement
Ethical clearance was obtained from the Institutional Ethical Committee with reference number (318/IEC/IGIMS/2022).
Conflicts of interest
None
Patient consent
Written informed consent was duly obtained.
Research Article: Case Report |
Subject:
Laboratory Sciences
Received: 2022/12/20 | Accepted: 2024/01/24 | Published: 2024/02/25 | ePublished: 2024/02/25
Received: 2022/12/20 | Accepted: 2024/01/24 | Published: 2024/02/25 | ePublished: 2024/02/25
References
1. Dimopoulos MA, Palumbo A, Delasalle KB, Alexaninan R. Primary plasma cell leukaemia. Br J Haematol. 1994;88(4):754-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Hovenga S, de Wolf JThM, Klip H, Vellenga E. Consolidation therapy with autologous stem cell transplantation in plasma cell leukemia after VAD, high-dose cyclophosphamide and EDAP courses: A report of three cases and a review of the literature. Bone Marrow Transplant. 1997;20(10):901-4. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Garcia-Sanz R, Orfao A, Gonzlez M, Tabernero MD, blade J, Moro MJ, et al. Primary Plasma Cell Leukemia: Clinical, Immunophenotypic, DNA Ploidy and Cytogenetic characteristics: Blood. 1999;93(3):1032-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Youssefi H, Ahnach M, Bendari M, Al Bouzidi A. Primary plasma cell leukemia revealed by mandibular lesion: a case report. 2021;13(12):e20148. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Costello R, Sainty D, Bouabdallah R, Fermand JP, Delmer A, Divine M, et al. Primary plasma cell leukemia: a report of 18 cases. Leuk Res. 2001;25(2): 103-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Mak YK, Chan CH, Chen YT, Lau SM, So CC, Wong KF. Consolidation therapy with autologous blood stem cell transplantation in a patient with primary plasma cell leukaemia. Clin Lab Haematol. 2003;25(1):55-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Raj RS, Najeeb S, Aruna R, Pavithran K, Thomas M. Primary plasma cell leukemia occurring in the young. Indian J Cancer. 2003;40(3):116-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Jain D, Singh T, Akhila L, Ghosh N. Primary plasma cell leukemia in a 30-year-old woman. Indian J Pathol Microbiol. 2008;51(3):456-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Swaminanthan N, Varadi G. Secondary Plasma cell leukemia: a case report .Cureus. 2020;12(6):e8693. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









 goums.ac.ir
goums.ac.ir yahoo.com
yahoo.com