Volume 17, Issue 6 (Nov-Dec 2023)
mljgoums 2023, 17(6): 23-26 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Esmaeili H, Shams Nateri S, Ebrahimi M. The high prevalent involvement of the left coronary artery in Kawasaki disease patients referred to Gorgan's Taleghani Hospital: A retrospective study. mljgoums 2023; 17 (6) :23-26
URL: http://mlj.goums.ac.ir/article-1-1434-en.html
URL: http://mlj.goums.ac.ir/article-1-1434-en.html
1- Congenital Malformations Research Center, Department of Pediatrics, Taleghani Medical Education Center, Golestan University of Medical Sciences, Gorgan, Iran
2- Children's Research Center, Golestan University of Medical Sciences, Gorgan, Iran , M1355ebrahimi@gmail.com
2- Children's Research Center, Golestan University of Medical Sciences, Gorgan, Iran , M1355ebrahimi@gmail.com
Full-Text [PDF 506 kb]
(162 Downloads)
| Abstract (HTML) (347 Views)
Full-Text: (53 Views)
Introduction
Kawasaki disease (KD) is a febrile systemic vasculitis spreading across developing countries, mainly affecting children under 5 years old (1). There are 4 stages of the disease: acute, subacute, collapsing, and chronic. Fevers of 39 °C, distinguishing the acute phase or higher, could be fatal for children (2). Diagnosis is based on clinical (3) and laboratory findings (2). After KD, the most common complication is coronary artery involvement, which can range from no evident involvement in the majority of patients to several large aneurysms (4).
The most severe consequence of KD is coronary artery lesions (CALs) (2,5), which account for around 15-20% of KD sequelae and can develop into significant coronary artery stenosis and ischemic heart disease (6). The first-line treatment of the disease includes intravenous injection (IV) of high doses of immunoglobulin (IVIG), along with aspirin (2). Coronary artery lesions decrease after treatment with IVIG with aspirin (7). However, treatment may be delayed due to different levels of diagnosis and therapeutics, and some patients may not respond to routine treatment regimens (8,9). The disease's management and monitoring depend on the severity and extent of coronary artery involvement. Children with KD-associated coronary artery aneurysms or obstructions require long-term drug treatment and monitoring (10). According to studies, KD has become more prevalent in recent years (11-13).
Given the significance of KD in children, its complications, and its increased incidence, it is critical to examine positive cases of the disease to assess its characteristics, risk factors, and complications, particularly coronary artery disease, which is a significant factor in Kawasaki-related mortality rates in children. According to Cheraghali et al., from 2005 to 2012, the prevalence of KD among children admitted to Gorgan (Iran) hospitals was 37.39% (14). Given the relatively high incidence of KD in children hospitalized at Gorgan's children's hospitals, it is critical to conduct a retrospective analysis to assess the prevalence of coronary artery-related sequelae. As a response, this study sought to investigate the medical histories of children with KD referred to Taleghani Hospital in Gorgan between 2007 and 2017 and emphasize the incidence of coronary artery disease and its contributing aspects.
Methods
In this retrospective study, patients referred to Taleghani Subspecialty Center during 2007-2017 who had clinical symptoms of KD were examined for disease frequency and demographic information.
Patients with symptoms including fever lasting more than 5 days, bilateral nonpurulent conjunctivitis, oral and pharyngeal mucosal changes (redness, dryness, cracked lips, strawberry tongue), limb involvement (swelling of hands and feet, redness of hands and feet, or scaling in the acute stage), skin rash, and unilateral cervical adenopathy larger than 1.5 cm were included in the study. Also, patients who had similar diseases with infectious causes or incomplete clinical information were excluded from the study.
The census approach was employed for sampling in this study. Thus, all eligible patients admitted to the hospital between 2007 and 2017 who had records in the hospital were chosen at random.
The current investigation was approved by the Ethics Committee, Golestan University of Medical Sciences, under the approval code of IR.GOUMS.REC.1400. As a retrospective study, the patients' parents were requested to provide their informed consent to use their child's medical records. Personal information gathered during the research is kept private.
Retrospective research was conducted on individuals diagnosed with KD by a pediatric cardiologist. A total of 108 patients met the inclusion criteria for the research. The information needed for the investigation was gathered from the patient's medical records. Patients' demographic data, such as age and sex, and paraclinical results, such as examination results, echocardiography and chest radiography reports, and treatments received, were thoroughly examined and extracted.
The information was imported into the SPSS v. 16 statistical software (SPSS Inc., Chicago, IL, USA). The chi-square test was performed to compare qualitative variables between groups. The student t test or one-way analysis of variance (ANOVA) was used to evaluate quantitative variables between groups. P-values of less than 0.05 with a 95% confidence level (CI) were considered significant.
Results
A total of 108 patients with a definitive diagnosis of KD, hospitalized in Gorgan Children's Hospital, were involved in this study from 2007-2007. Sixty-three patients (58.3%) were male, and 45 patients (41.7%) were female. The mean age of the subjects was 20.83 ± 26.87 months. The demographic information of the patients is shown in Table 1. The patients were evaluated for body temperature and duration of fever at admission. At the time of admission, the mean body temperature was 38.5 °C (38.5 °C and 39 °C in the boys and girls, respectively). However, female patients showed higher mean body temperature.
Clinical manifestations of patients at the time of admission, including conjunctivitis, mucosal involvement, skin involvement, organ involvement, and lymphadenopathy, were obtained from their records (Figure 1). No significant differences were observed between the two sexes based on clinical manifestations (P-value <0.05).
Laboratory radiological records of the patients at admission were extracted and analyzed. The results showed that the mean hemoglobin levels, white blood cell count, and platelet count were 1.33 ± 9.89, 5.35 ± 13.04, and 19.88 ± 426.61, respectively (Table 1). In addition, the results indicated higher erythrocyte sedimentation rate (ESR) levels in female patients. (P-value = 0.008).

Out of 108 patients, 21 (19.4%) had abnormal echocardiography, of whom 11/108 patients (17.5%) were male and 10/108 patients (22.2%) were female. The patterns of coronary artery involvement were also determined in the patients; 14/108 patients (13%) had involvement of the left coronary artery, 4/108 patients (3.7%) had involvement of 2 coronary arteries, 1/108 patient (0.9%) showed involvement of all 3 coronary arteries, and 1/108 patient (0.9%) had valvular dysfunction. The patients showed different patterns of involvement in echocardiography (Table 2).
The relationship between variables was measured to assess the risk factors for coronary artery involvement and abnormal echocardiographic findings. The results showed no significant relationship between clinical manifestations and abnormal echocardiographic findings (Table 3).
The relationship between laboratory findings at the time of admission and abnormal findings in echocardiography was examined. The results showed no significant relationship between the studied variables and abnormal findings in echocardiography (Table 4).
The highest incidence of coronary artery disease, with 14/21 cases (66.67%), was related to the left main coronary artery, followed by 4/21 cases (19.05%) related to simultaneous involvement of the left and right coronary arteries (P-value = 0.000). Also, the results demonstrated that ectasia pattern, aneurysm, and dilation had the highest frequency in the vascular involvement pattern in echocardiography (P-value = 0.000) (Figure 2).

Discussion
The first case of KD was described in the 1960s by Tomisaku Kawasaki (15). The severity of coronary artery lesions measures prolonged prognosis. Therefore, KD is currently the leading cause of acquired heart disease in developed countries (9,16). This retrospective study aimed to evaluate the frequency of coronary artery lesions in Golestan Province and study the clinical factors observed in patients referred to Taleghani Hospital during 2007-2017.
The coronary artery is the most common site of KD (17). Narrowing or obstructing the lumen most likely involves the LCA following the right coronary artery (18). The findings of the present study support the highly prevalent involvement of LCA. Additionally, it was observed that > 19% of the cases were related to simultaneous involvement of the left and right main coronary arteries. On the other hand, the pattern of vascular involvement in echocardiography showed ectasia, aneurysm, and dilation with the highest frequency, respectively.
Most of the current study records comprised children < 3 years old. This was consistent with a retrospective study in northern Iran, showing that most patients with KD in northern Iran are between 1 and 3 years old and are mostly boys (19). In addition, all patients were treated with a single dose of intravenous immunoglobulin along with a high-dose salicylic acid, as was reported before (8,9,17,18,20).
Different geographical regions may affect the incidence of KD-associated coronary artery lesions. From 2004 to 2014 in Canada, KD-related coronary artery lesions affected 3.5% of all patients (21). In the United States, 3.20-2.25% of patients with KD suffered from coronary artery aneurysms (22,23). In addition, a study in Australia found that the incidence of coronary artery dilatation was 16.7% (24). The range of KD-associated coronary artery complications in Asian countries is around 3% to 30% (18,25-28). Further studies have been conducted in Iran. In a study of Mazandaran Province, 25% of cases with KD had heart disorders (19). In studies conducted in Yazd (29), Urmia (30), and Ilam (31), 39.5%, 12%, and 32.9% of cases had KD-coronary artery diseases, respectively. The present study's findings demonstrated KD-associated coronary artery in 19.4% of patients. Differences in reported coronary artery symptoms could be due to different diagnostic levels, differences in treatment protocols, or delays in diagnosis and
Coronary artery lesions vary with sex and age, and boys and infants are more prone to KD-associated coronary artery lesions (28). However, pathological factors have not yet been identified. It was found that at the start of KD, there was an increase in ESR, C-reactive protein (CRP), white blood cell (WBC) count, liver enzymes, and a drop in hemoglobin and albumin levels (32). However, we found no association between the laboratory findings, including WBC count, hemoglobulin, platelet, CPR, ESR, albumin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and coronary artery; similar results were reported Rahbarimanesh et al. (32).
The development of Kawasaki-associated coronary artery lesions is a chronic process that requires close monitoring of patients, as some vascular problems can develop later, even after the coronary aneurysm has disappeared. In some cases, no coronary artery lesions are found in the acute phase, which is generally a good prognosis. However, long-term cardiovascular risk is still possible. It is challenging to know and justify the processes of coronary artery involvement over a long period because follow-up data have so far been limited to monitoring middle-aged and elderly patients with a high prevalence of cardiovascular disease (33).
Conclusion
Kawasaki disease-associated coronary artery complications are more frequent in children under 3 years old, especially boys, in Gorgan. The left coronary artery is the most common site of coronary artery complication in KD children in Gorgan. The physicians can use the findings for a better prognosis of patients with KD.
Acknowledgement
Not applicable.
Funding sources
Not applicable.
Ethical statement
The Ethics Committee at Golestan University of Medical Sciences has approved the study under the approval code of IR.GOUMS.REC.1400.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
All the authors have participated in one or more parts of the present study, including data gathering, data entry, data analysis, writing the first draft of the manuscript, and editing the manuscript.
Kawasaki disease (KD) is a febrile systemic vasculitis spreading across developing countries, mainly affecting children under 5 years old (1). There are 4 stages of the disease: acute, subacute, collapsing, and chronic. Fevers of 39 °C, distinguishing the acute phase or higher, could be fatal for children (2). Diagnosis is based on clinical (3) and laboratory findings (2). After KD, the most common complication is coronary artery involvement, which can range from no evident involvement in the majority of patients to several large aneurysms (4).
The most severe consequence of KD is coronary artery lesions (CALs) (2,5), which account for around 15-20% of KD sequelae and can develop into significant coronary artery stenosis and ischemic heart disease (6). The first-line treatment of the disease includes intravenous injection (IV) of high doses of immunoglobulin (IVIG), along with aspirin (2). Coronary artery lesions decrease after treatment with IVIG with aspirin (7). However, treatment may be delayed due to different levels of diagnosis and therapeutics, and some patients may not respond to routine treatment regimens (8,9). The disease's management and monitoring depend on the severity and extent of coronary artery involvement. Children with KD-associated coronary artery aneurysms or obstructions require long-term drug treatment and monitoring (10). According to studies, KD has become more prevalent in recent years (11-13).
Given the significance of KD in children, its complications, and its increased incidence, it is critical to examine positive cases of the disease to assess its characteristics, risk factors, and complications, particularly coronary artery disease, which is a significant factor in Kawasaki-related mortality rates in children. According to Cheraghali et al., from 2005 to 2012, the prevalence of KD among children admitted to Gorgan (Iran) hospitals was 37.39% (14). Given the relatively high incidence of KD in children hospitalized at Gorgan's children's hospitals, it is critical to conduct a retrospective analysis to assess the prevalence of coronary artery-related sequelae. As a response, this study sought to investigate the medical histories of children with KD referred to Taleghani Hospital in Gorgan between 2007 and 2017 and emphasize the incidence of coronary artery disease and its contributing aspects.
Methods
In this retrospective study, patients referred to Taleghani Subspecialty Center during 2007-2017 who had clinical symptoms of KD were examined for disease frequency and demographic information.
Patients with symptoms including fever lasting more than 5 days, bilateral nonpurulent conjunctivitis, oral and pharyngeal mucosal changes (redness, dryness, cracked lips, strawberry tongue), limb involvement (swelling of hands and feet, redness of hands and feet, or scaling in the acute stage), skin rash, and unilateral cervical adenopathy larger than 1.5 cm were included in the study. Also, patients who had similar diseases with infectious causes or incomplete clinical information were excluded from the study.
The census approach was employed for sampling in this study. Thus, all eligible patients admitted to the hospital between 2007 and 2017 who had records in the hospital were chosen at random.
The current investigation was approved by the Ethics Committee, Golestan University of Medical Sciences, under the approval code of IR.GOUMS.REC.1400. As a retrospective study, the patients' parents were requested to provide their informed consent to use their child's medical records. Personal information gathered during the research is kept private.
Retrospective research was conducted on individuals diagnosed with KD by a pediatric cardiologist. A total of 108 patients met the inclusion criteria for the research. The information needed for the investigation was gathered from the patient's medical records. Patients' demographic data, such as age and sex, and paraclinical results, such as examination results, echocardiography and chest radiography reports, and treatments received, were thoroughly examined and extracted.
The information was imported into the SPSS v. 16 statistical software (SPSS Inc., Chicago, IL, USA). The chi-square test was performed to compare qualitative variables between groups. The student t test or one-way analysis of variance (ANOVA) was used to evaluate quantitative variables between groups. P-values of less than 0.05 with a 95% confidence level (CI) were considered significant.
Results
A total of 108 patients with a definitive diagnosis of KD, hospitalized in Gorgan Children's Hospital, were involved in this study from 2007-2007. Sixty-three patients (58.3%) were male, and 45 patients (41.7%) were female. The mean age of the subjects was 20.83 ± 26.87 months. The demographic information of the patients is shown in Table 1. The patients were evaluated for body temperature and duration of fever at admission. At the time of admission, the mean body temperature was 38.5 °C (38.5 °C and 39 °C in the boys and girls, respectively). However, female patients showed higher mean body temperature.
Clinical manifestations of patients at the time of admission, including conjunctivitis, mucosal involvement, skin involvement, organ involvement, and lymphadenopathy, were obtained from their records (Figure 1). No significant differences were observed between the two sexes based on clinical manifestations (P-value <0.05).
Laboratory radiological records of the patients at admission were extracted and analyzed. The results showed that the mean hemoglobin levels, white blood cell count, and platelet count were 1.33 ± 9.89, 5.35 ± 13.04, and 19.88 ± 426.61, respectively (Table 1). In addition, the results indicated higher erythrocyte sedimentation rate (ESR) levels in female patients. (P-value = 0.008).
Table 1. The demographical and fever information of patients with Kawasaki disease and the differences between the two sexes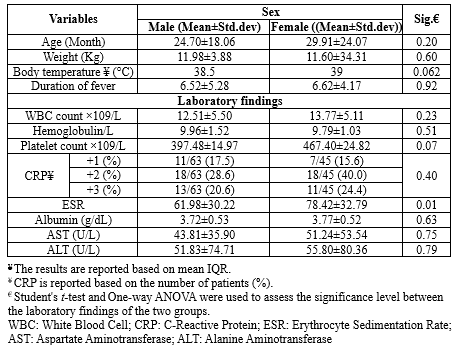 |

Out of 108 patients, 21 (19.4%) had abnormal echocardiography, of whom 11/108 patients (17.5%) were male and 10/108 patients (22.2%) were female. The patterns of coronary artery involvement were also determined in the patients; 14/108 patients (13%) had involvement of the left coronary artery, 4/108 patients (3.7%) had involvement of 2 coronary arteries, 1/108 patient (0.9%) showed involvement of all 3 coronary arteries, and 1/108 patient (0.9%) had valvular dysfunction. The patients showed different patterns of involvement in echocardiography (Table 2).
Table 2. Echocardiographic findings of patients with Kawasaki disease based on sex |
|
Table 3. Association of clinical manifestations of patients with Kawasaki disease with echocardiography findings
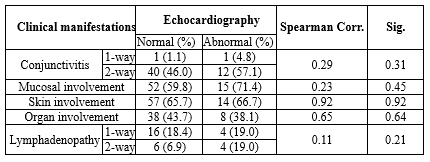 |
Table 4. Laboratory findings associated with echocardiographic findings |

Discussion
The first case of KD was described in the 1960s by Tomisaku Kawasaki (15). The severity of coronary artery lesions measures prolonged prognosis. Therefore, KD is currently the leading cause of acquired heart disease in developed countries (9,16). This retrospective study aimed to evaluate the frequency of coronary artery lesions in Golestan Province and study the clinical factors observed in patients referred to Taleghani Hospital during 2007-2017.
The coronary artery is the most common site of KD (17). Narrowing or obstructing the lumen most likely involves the LCA following the right coronary artery (18). The findings of the present study support the highly prevalent involvement of LCA. Additionally, it was observed that > 19% of the cases were related to simultaneous involvement of the left and right main coronary arteries. On the other hand, the pattern of vascular involvement in echocardiography showed ectasia, aneurysm, and dilation with the highest frequency, respectively.
Most of the current study records comprised children < 3 years old. This was consistent with a retrospective study in northern Iran, showing that most patients with KD in northern Iran are between 1 and 3 years old and are mostly boys (19). In addition, all patients were treated with a single dose of intravenous immunoglobulin along with a high-dose salicylic acid, as was reported before (8,9,17,18,20).
Different geographical regions may affect the incidence of KD-associated coronary artery lesions. From 2004 to 2014 in Canada, KD-related coronary artery lesions affected 3.5% of all patients (21). In the United States, 3.20-2.25% of patients with KD suffered from coronary artery aneurysms (22,23). In addition, a study in Australia found that the incidence of coronary artery dilatation was 16.7% (24). The range of KD-associated coronary artery complications in Asian countries is around 3% to 30% (18,25-28). Further studies have been conducted in Iran. In a study of Mazandaran Province, 25% of cases with KD had heart disorders (19). In studies conducted in Yazd (29), Urmia (30), and Ilam (31), 39.5%, 12%, and 32.9% of cases had KD-coronary artery diseases, respectively. The present study's findings demonstrated KD-associated coronary artery in 19.4% of patients. Differences in reported coronary artery symptoms could be due to different diagnostic levels, differences in treatment protocols, or delays in diagnosis and
Coronary artery lesions vary with sex and age, and boys and infants are more prone to KD-associated coronary artery lesions (28). However, pathological factors have not yet been identified. It was found that at the start of KD, there was an increase in ESR, C-reactive protein (CRP), white blood cell (WBC) count, liver enzymes, and a drop in hemoglobin and albumin levels (32). However, we found no association between the laboratory findings, including WBC count, hemoglobulin, platelet, CPR, ESR, albumin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and coronary artery; similar results were reported Rahbarimanesh et al. (32).
The development of Kawasaki-associated coronary artery lesions is a chronic process that requires close monitoring of patients, as some vascular problems can develop later, even after the coronary aneurysm has disappeared. In some cases, no coronary artery lesions are found in the acute phase, which is generally a good prognosis. However, long-term cardiovascular risk is still possible. It is challenging to know and justify the processes of coronary artery involvement over a long period because follow-up data have so far been limited to monitoring middle-aged and elderly patients with a high prevalence of cardiovascular disease (33).
Conclusion
Kawasaki disease-associated coronary artery complications are more frequent in children under 3 years old, especially boys, in Gorgan. The left coronary artery is the most common site of coronary artery complication in KD children in Gorgan. The physicians can use the findings for a better prognosis of patients with KD.
Acknowledgement
Not applicable.
Funding sources
Not applicable.
Ethical statement
The Ethics Committee at Golestan University of Medical Sciences has approved the study under the approval code of IR.GOUMS.REC.1400.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
All the authors have participated in one or more parts of the present study, including data gathering, data entry, data analysis, writing the first draft of the manuscript, and editing the manuscript.
Research Article: Research Article |
Subject:
Biochemistry
Received: 2021/09/21 | Accepted: 2022/08/3 | Published: 2024/02/26 | ePublished: 2024/02/26
Received: 2021/09/21 | Accepted: 2022/08/3 | Published: 2024/02/26 | ePublished: 2024/02/26
References
1. Lim EJ, Aris IM, Choo J, Wong TY, Li LJ. Association between Coronary Artery Measurements and Retinal Microvasculature in Children with New Onset of Kawasaki Disease. Sci Rep. 2019;9(1):16714. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Shiari R. Kawasaki disease; A review article. Arch Pediatr Infect Dis. 2013;2(1):154-9. [View at Publisher] [DOI] [Google Scholar]
3. Prata A. Clinical and epidemiological aspects of Chagas disease. Lancet Infect Dis. 2001;1(2):92-100. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. McCrindle BW, Li JS, Minich LLA, Colan SD, Atz AM, Takahashi M, et al. Coronary artery involvement in children with Kawasaki disease: Risk factors from analysis of serial normalized measurements. Circulation. 2007;116(2):174-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Mammadov G, Liu HH, Chen WX, Fan GZ, Li RX, Liu FF, et al. Hepatic dysfunction secondary to Kawasaki disease: characteristics, etiology and predictive role in coronary artery abnormalities. Clin Exp Med. 2020;20(1):21-30. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Yang M, Pei Q, Zhang J, Weng H, Jing F, Yi Q. Association between adropin and coronary artery lesions in children with Kawasaki disease. Eur J Pediatr. 2021;180(7):2253-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Furusho K, Kamiya T, Nakano H, Kiyosawa N, Shinomiya K, Hayashidera T, et al. High-Dose Intravenous Gammaglobulin for Kawasaki Disease. Lancet. 1984;2(8411):1055-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Kobayashi T, Saji T, Otani T, Takeuchi K, Nakamura T, Arakawa H, et al. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): A randomised, open-label, blinded-endpoints trial. Lancet. 2012;379(9826):1613-20. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Tremoulet AH, Jain S, Jaggi P, Jimenez-Fernandez S, Pancheri JM, Sun X, et al. Infliximab for intensification of primary therapy for Kawasaki disease: A phase 3 randomised, double-blind, placebo-controlled trial. Lancet. 2014;383(9930):1731-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Yılmazer MM, Öner T, Gökalp S, Doksöz Ö, Güven B, Vupa-Çilengiroğlu Ö, et al. Risk factors for persistence of coronary artery abnormalities in Turkish children with Kawasaki disease. Turk J Pediatr. 2015;57(3):248-53. [View at Publisher] [PMID] [Google Scholar]
11. Nakamura Y, Yashiro M, Uehara R, Oki I, Kayaba K, Yanagawa H. Increasing incidence of Kawasaki disease in Japan: Nationwide survey. Pediatr Int. 2008;50(3):287-90. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Belay ED, Maddox RA, Holman RC, Curns AT, Ballah K, Schonberger LB. Kawasaki syndrome and risk factors for coronary artery abnormalities: United States, 1994-2003. Pediatr Infect Dis J. 2006;25(3):245-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Ghelani SJ, Kwatra NS, Spurney CF. Can coronary artery involvement in kawasaki disease be predicted? Diagnostics. 2013;3(2):232-43. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Cheraghali F, Hajimoradloo N, Roshandel G, Meftah M, Azadfar S. Prevalence of Kawasaki Disease in Children Admitted to Taleghani Medical Center in Gorgan, Iran. J Clin Basic Res. 2018;2(4):54-9. [View at Publisher] [DOI] [Google Scholar]
15. Kawasaki T. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Jpn J Allergy. 1967;16(3):178-222. [View at Publisher] [PMID] [Google Scholar]
16. Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004;110(17):2747-71. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Yonesaka S, Takahashi T, Eto S, Sato T, Otani K, Ueda T, et al. Biopsy-proven myocardial sequels in Kawasaki disease with giant coronary aneurysms. Cardiol Young. 2010;20(6):602-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Chen JJ, Ma XJ, Liu F, Yan WL, Huang MR, Huang M, et al. Epidemiologic features of Kawasaki disease in Shanghai from 2008 Through 2012. Pediatr Infect Dis J. 2016;35(1):7-12. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Saffar MJ, Reshidighader F. Kawasaki disease in East Mazandaran, Islamic Republic of Iran, 1997-2002. East Mediterr Health J. 2005;11(1-2):28-35. [View at Publisher] [PMID] [Google Scholar]
20. Türkuçar S, Yıldız K, Acarı C, Dundar HA, Kır M, Ünsal E. Risk factors of intravenous immunoglobulin resistance and coronary arterial lesions in Turkish children with Kawasaki disease. Turk J Pediatr. 2020;62(1):1-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Manlhiot C, O'Shea S, Bernknopf B, LaBelle M, Chahal N, Dillenburg RF, et al. Epidemiology of Kawasaki Disease in Canada 2004 to 2014: Comparison of Surveillance Using Administrative Data vs Periodic Medical Record Review. Can J Cardiol. 2018;34(3):303-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Okubo Y, Nochioka K, Sakakibara H, Testa M, Sundel RP. National survey of pediatric hospitalizations due to Kawasaki disease and coronary artery aneurysms in the USA. Clin Rheumatol. 2017;36(2):413-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Dominguez SR, Anderson MS, El-Adawy M, Glodé MP. Preventing coronary artery abnormalities: A need for earlier diagnosis and treatment of Kawasaki disease. Pediatr Infect Dis J. 2012;31(12):1217-20. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Saundankar J, Yim D, Itotoh B, Payne R, Maslin K, Jape G, et al. The epidemiology and clinical features of kawasaki disease in australia. Pediatrics. 2014;133(4):e1009-14. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Skochko SM, Jain S, Sun X, Sivilay N, Kanegaye JT, Pancheri J, et al. Kawasaki Disease Outcomes and Response to Therapy in a Multiethnic Community: A 10-Year Experience. J Pediatr. 2018;203:408-15. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Lue HC, Chen LR, Lin MT, Chang LY, Wang JK, Lee CY, et al. Epidemiological features of Kawasaki disease in Taiwan, 1976-2007: Results of five nationwide questionnaire hospital surveys. Pediatr Neonatol. 2014;55(2):92-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Kim GB, Park S, Eun LY, Han JW, Lee SY, Yoon KL, et al. Epidemiology and clinical features of Kawasaki disease in South Korea, 2012-2014. Pediatr Infect Dis J. 2017;36(5):482-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Makino N, Nakamura Y, Yashiro M, Ae R, Tsuboi S, Aoyama Y, et al. Descriptive epidemiology of Kawasaki disease in Japan, 2011-2012: From the results of the 22nd nationwide survey. J Epidemiol. 2015;25(3):239-45. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Akhavan Karbasi S, Golestan M, Roozbeh P. A 10-year study on the prevalence of cardiovascular affliction among Kawasaki patients in Yazd, Iran. Feyz. 2009;13(1):55-8. [View at Publisher] [Google Scholar]
30. Mahmoudzadeh H, Nikibakhsh AA, Gheibi SS, Aghayar Makoui A. A survey on kawasaki disease in imam khomeini hospital, Urmia. Studies in Medical Sciences. 2008;19(3):236-41. [View at Publisher] [Google Scholar]
31. Amirimoghadam Z, Molaee S, Rezazadeh M, Ghaneei Z, Babaei haidar abadi A, Hemati R. Assessment Heart Involvement in Patients With Kawasaki Disease. J Ilam Univ Med Sci. 2013;21(1):129-34. [View at Publisher] [Google Scholar]
32. Rahbarimanesh A, Salamati P, Ghafourian S, Zekavat M. Relationship between ESR, CRP, platelet count and coronary artery disease in Kawasaki disease. Iranian Journal of Pediatrics. 2005;15(2):139-44. [View at Publisher] [Google Scholar]
33. Zhang D, Liu L, Huang X, Tian J. Insights Into Coronary Artery Lesions in Kawasaki Disease. Front Pediatr. 2020;8:493. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.







