Volume 15, Issue 6 (Special issue (Nov-Dec) 2021)
mljgoums 2021, 15(6): 23-30 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Chakroun A, Baccouche H, Mahjoub S, Ben Romdhane N. Assessment of Peripheral Blood Lymphocytosis in Adults: Determination of Thresholds for Differential Diagnosis between Clonal and Reactive Lymphocytosis. mljgoums 2021; 15 (6) :23-30
URL: http://mlj.goums.ac.ir/article-1-1411-en.html
URL: http://mlj.goums.ac.ir/article-1-1411-en.html
1- La Rabta University Hospital, Hematology Department, La Rabta University Hospital, Tunis, Tunisia And Faculty of Medicine of Tunis, Tunis University El Manar, Tunis, Tunisia , aya.chakroun@fmt.utm.tn
2- La Rabta University Hospital, Hematology Department, La Rabta University Hospital, Tunis, Tunisia And Faculty of Medicine of Tunis, Tunis University El Manar, Tunis, Tunisia
2- La Rabta University Hospital, Hematology Department, La Rabta University Hospital, Tunis, Tunisia And Faculty of Medicine of Tunis, Tunis University El Manar, Tunis, Tunisia
Full-Text [PDF 718 kb]
(569 Downloads)
| Abstract (HTML) (1965 Views)
INTRODUCTION
Lymphocytosis is a common observation in laboratory and clinical practice. Lymphocytosis of benign origin is called reactive lymphocytosis (RL), but it could also be caused by infections with viral (Epstein-Barr virus, cytomegalovirus), bacterial (Mycoplasma pneumoniae, Treponema pallidum) or parasitic (Toxoplasma gondii) agents. In these situations, lymphocytosis usually normalizes after resolution of the antigenic stimulus (1). Endocrine disorders (thyrotoxicosis), autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, etc.), smoking, splenectomy or some medications may also induce RL (1, 2). Unlike RL, malignant lymphocytosis or clonal lymphocytosis (CL) is less common and include acute lymphoblastic leukemia and chronic lymphoproliferative disorders (LPD). The World Health Organization classification of lymphoid neoplasia in 2016recognizes several entities according to their clinical, morphological, immunophenotypic, cytogenetic and molecular characteristics (3).
It is important for biologists to be able to distinguish RL from CL. Both the International Society of Laboratory Hematology (ISLH) (4) and the Francophone Group of Cellular Hematology (GFHC) (5) recommend the analysis of blood smears for peripheral blood lymphocytosis> 5 G/l. Although blood smear review often allows the distinction between CL and RL, this process can be less efficient in cases of moderate lymphocytosis (6). Moreover, there are morphological features that could be confusing such as the presence of atypical lymphocytes encountered either during viral infections or during leukemia (7).
Meanwhile, advances in hematology analyzers have improved the ability to detect lymphocyte population’s changes in peripheral blood samples through the use of hematologic research parameters such as the high fluorescence lymphocyte cell (HFLC) count. This structural parameter identifies activated lymphocytes in a six-part differential channel using a flow cytometry principle (8). However, HFLC is not yet commonly used, probably because of lack of specific reference ranges and quality control as well as the lack of data regarding its diagnostic value (8, 9).Moreover, hematology analyzers can generate morphological flags that may encourage a blood smear review. However, these flags may have low sensitivity and specificity.
Among conventional hematologic parameters, absolute lymphocytes count (ALC) was reported to be helpful for screening LPD (10, 11). Some algorithms have been proposed to discriminate CL from RL but none has integrated HFLC (10-13). The present study aimed to evaluate performance of the extended complete blood count (CBC) parameters including HFLC and morphological flags on Sysmex XT4000i® analyzer and to determine thresholds of discriminating CL and RL variables. Ultimately, we proposed an algorithm for moderate lymphocytosis in adults.
MATERIALS AND METHODS
Samples collection
Blood samples from adult patients (age>18 years) with absolute lymphocytosis (> 5G/l) were prospectively collected over a 4-month period. The specimens were sent from inpatient and outpatient departments to the Hematology Laboratory of our University Hospital. Blood was collected in standard K2EDTA tubes. Then, CBC including HFLC analysis and blood smear preparation was performed using the Sysmex XT4000i® within four hours of sample collection. Samples from the emergency department were not included since they were performed using another analyzer.
Instrument
The Sysmex XT4000i® (Sysmex Corporation, Kobe, Japan) is a hematology analyzer that performs based on impedance method and fluorescence flow cytometry using a laser light after treatment of the cells with lysing reagents and specific fluorescent dyes that bind to nucleic acids and cytoplasmic organelles. The forward-scattered light is proportional to the cell size. The side-scattered light is proportional to the internal structure and complexity of the cell. The lateral fluorescent light is related to RNA and DNA concentration in the cell. Data obtained from the analyzer are presented through scattergram. Extended information processing unit provides data on HFLC, which is quantified by the analyzer’s Diff channel and expressed as a percentage of the total number of leukocytes. This parameter reflects a high RNA content cells, such as activated cells i.e. B lymphocytes secreting antibodies or plasma cells. The Sysmex analyzer can also detect the presence of circulating abnormal cells and trigger morphological flags such as abnormal lymphocytes or blasts flag (AbnLym/BL) as well as abnormal scattergram (abnormal scatter).In our study, the analyzer operated in routine mode according to the manufacturer’s instructions. Three levels of internal quality controls were regularly evaluated. Numerical data and qualitative flags were recorded and studied for all samples.
Morphological study
Blood films were prepared and stained with May-Grünwald Giemsa staining. Smears were reviewed for cytological features by an expert hematologist who was blind to patients’ demographics and clinical information. Samples exhibiting nucleated red blood cells were excluded from the study. The evaluated morphological criterion was the presence of atypical lymphocytes and smudge cells.
Population data and diagnostic criteria
Patients’ demographic, clinical and laboratory data were obtained from medical records. Two groups of CL and RL were formed. The clonal origin of lymphocytosis was confirmed by flow cytometry and/or histological data (if bone marrow biopsy had been performed). In the CL group, all patients were diagnosed within the two years preceding the study and were not on chemotherapy at the time of sample collection. The reactive origin of lymphocytosis was defined as a decrease in lymphocytosis during hospitalization or the demonstration of clinical or biological pattern showing recent infection.
Statistical analysis
All data were analyzed with the SPSS 19.0 software. The Shapiro-Wilk test was used to determine normal distribution of continuous variables. Unpaired Student t-test was used to compare age and absolute lymphocytes count between the two groups. The Mann-Whitney U test was used to compare other continuous variables. Qualitative morphological flags were compared using the Fisher exact test. Receiver operating characteristic (ROC) curves were generated. The areas under the curve (AUC) were analyzed and values above 0.7 indicated favorable diagnostic accuracy. Discriminatory parameters, optimal cut-offs, sensitivity and specificity were established using the ROC curve analysis. The accuracy was calculated by 2 × 2 truth tables as follows: Accuracy = (true negative + true positive)/(true negative + true positive + false negative+ false positive). A p-value of < 0.05 was considered statistically significant.
Ethical considerations
This study was carried out on routine samples collected for diagnostic procedures. Parameters were obtained without any additional cost and without compromising the results of the clinical analysis. The study protocol was in accordance with the Declaration of Helsinki. The ethical clearance for this study was obtained from the local institutional review board.
RESULTS
General characteristics of the subjects
Ninety samples (lymphocytosis> 5G/L) from 67 patients were collected during the study period. Five samples were excluded because of interference due to the presence of nucleated red blood cells in the blood films. Overall, 85 samples were divided into two groups of CL (n=51) and RL (n=34).There were 38 cases of chronic lymphocytic leukemia (CLL), 12 cases of LPD non-CLL and one case of acute lymphoblastic leukemia. Demographic characteristics and extended CBC findings of the two groups are presented in table1.
Table 1.Comparative analysis of clinical and hematological parameters in CL and RL groups
Full-Text: (1743 Views)
ABSTRACT
Background and objectives: Differential diagnosis between clonal lymphocytosis (CL) and reactive lymphocytosis (RL) is often established through blood smear examination but with some limitations. We aimed to evaluate ability of clinical data and extended-cells blood count (CBC) parameters to discriminate CL from RL and to establish a decision-making algorithm for moderate lymphocytosis in adults.
Methods: A total of 85 samples were collected from adults with absolute lymphocytescount of >5G/l. The samples were divided into RL group (n=34) and newly diagnosed CL group (n=51).Demographic data, CBC parameters including high fluorescence lymphocytes cells percentage (HFLC%) and abnormal lymphocytes or blasts (’AbnLym/BL’’) morphological flag were evaluated for each study group. New threshold for discriminating parameters were determined using receiver operating characteristic (ROC) curves and used in an algorithm for moderate lymphocytosis.
Results: Age, high lymphocytes count and the presence of the ’AbnLym/BL’’ flag and low HFLC% were predictor of malignant lymphocytosis. Age threshold of 62.5 years and absolute lymphocytes count of > 10.47 G/l were highly effective in CL detection with area under the ROC curve of 0.9 and 0.99, respectively. In addition, HFLC% showed an area under the ROC curve of 0.71. Considering ALC threshold of 10.47 G/l alone, a sensitivity of 96.7% and a specificity of 100 % were achieved. For moderate lymphocytosis ranging between 5 and 10.47G/l, no false positive or negative result was detected when we considered both the proposed ALC and age cut-offs.
Conclusion: A combination threshold for ALC and age appears to be helpful for screening CL, especially in moderate lymphocytosis for both laboratory and clinical routine practice.
Keywords: Hematology analyzer, Lymphoproliferative disorders, Lymphocytosis, Discrimination power
Background and objectives: Differential diagnosis between clonal lymphocytosis (CL) and reactive lymphocytosis (RL) is often established through blood smear examination but with some limitations. We aimed to evaluate ability of clinical data and extended-cells blood count (CBC) parameters to discriminate CL from RL and to establish a decision-making algorithm for moderate lymphocytosis in adults.
Methods: A total of 85 samples were collected from adults with absolute lymphocytescount of >5G/l. The samples were divided into RL group (n=34) and newly diagnosed CL group (n=51).Demographic data, CBC parameters including high fluorescence lymphocytes cells percentage (HFLC%) and abnormal lymphocytes or blasts (’AbnLym/BL’’) morphological flag were evaluated for each study group. New threshold for discriminating parameters were determined using receiver operating characteristic (ROC) curves and used in an algorithm for moderate lymphocytosis.
Results: Age, high lymphocytes count and the presence of the ’AbnLym/BL’’ flag and low HFLC% were predictor of malignant lymphocytosis. Age threshold of 62.5 years and absolute lymphocytes count of > 10.47 G/l were highly effective in CL detection with area under the ROC curve of 0.9 and 0.99, respectively. In addition, HFLC% showed an area under the ROC curve of 0.71. Considering ALC threshold of 10.47 G/l alone, a sensitivity of 96.7% and a specificity of 100 % were achieved. For moderate lymphocytosis ranging between 5 and 10.47G/l, no false positive or negative result was detected when we considered both the proposed ALC and age cut-offs.
Conclusion: A combination threshold for ALC and age appears to be helpful for screening CL, especially in moderate lymphocytosis for both laboratory and clinical routine practice.
Keywords: Hematology analyzer, Lymphoproliferative disorders, Lymphocytosis, Discrimination power
INTRODUCTION
Lymphocytosis is a common observation in laboratory and clinical practice. Lymphocytosis of benign origin is called reactive lymphocytosis (RL), but it could also be caused by infections with viral (Epstein-Barr virus, cytomegalovirus), bacterial (Mycoplasma pneumoniae, Treponema pallidum) or parasitic (Toxoplasma gondii) agents. In these situations, lymphocytosis usually normalizes after resolution of the antigenic stimulus (1). Endocrine disorders (thyrotoxicosis), autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, etc.), smoking, splenectomy or some medications may also induce RL (1, 2). Unlike RL, malignant lymphocytosis or clonal lymphocytosis (CL) is less common and include acute lymphoblastic leukemia and chronic lymphoproliferative disorders (LPD). The World Health Organization classification of lymphoid neoplasia in 2016recognizes several entities according to their clinical, morphological, immunophenotypic, cytogenetic and molecular characteristics (3).
It is important for biologists to be able to distinguish RL from CL. Both the International Society of Laboratory Hematology (ISLH) (4) and the Francophone Group of Cellular Hematology (GFHC) (5) recommend the analysis of blood smears for peripheral blood lymphocytosis> 5 G/l. Although blood smear review often allows the distinction between CL and RL, this process can be less efficient in cases of moderate lymphocytosis (6). Moreover, there are morphological features that could be confusing such as the presence of atypical lymphocytes encountered either during viral infections or during leukemia (7).
Meanwhile, advances in hematology analyzers have improved the ability to detect lymphocyte population’s changes in peripheral blood samples through the use of hematologic research parameters such as the high fluorescence lymphocyte cell (HFLC) count. This structural parameter identifies activated lymphocytes in a six-part differential channel using a flow cytometry principle (8). However, HFLC is not yet commonly used, probably because of lack of specific reference ranges and quality control as well as the lack of data regarding its diagnostic value (8, 9).Moreover, hematology analyzers can generate morphological flags that may encourage a blood smear review. However, these flags may have low sensitivity and specificity.
Among conventional hematologic parameters, absolute lymphocytes count (ALC) was reported to be helpful for screening LPD (10, 11). Some algorithms have been proposed to discriminate CL from RL but none has integrated HFLC (10-13). The present study aimed to evaluate performance of the extended complete blood count (CBC) parameters including HFLC and morphological flags on Sysmex XT4000i® analyzer and to determine thresholds of discriminating CL and RL variables. Ultimately, we proposed an algorithm for moderate lymphocytosis in adults.
MATERIALS AND METHODS
Samples collection
Blood samples from adult patients (age>18 years) with absolute lymphocytosis (> 5G/l) were prospectively collected over a 4-month period. The specimens were sent from inpatient and outpatient departments to the Hematology Laboratory of our University Hospital. Blood was collected in standard K2EDTA tubes. Then, CBC including HFLC analysis and blood smear preparation was performed using the Sysmex XT4000i® within four hours of sample collection. Samples from the emergency department were not included since they were performed using another analyzer.
Instrument
The Sysmex XT4000i® (Sysmex Corporation, Kobe, Japan) is a hematology analyzer that performs based on impedance method and fluorescence flow cytometry using a laser light after treatment of the cells with lysing reagents and specific fluorescent dyes that bind to nucleic acids and cytoplasmic organelles. The forward-scattered light is proportional to the cell size. The side-scattered light is proportional to the internal structure and complexity of the cell. The lateral fluorescent light is related to RNA and DNA concentration in the cell. Data obtained from the analyzer are presented through scattergram. Extended information processing unit provides data on HFLC, which is quantified by the analyzer’s Diff channel and expressed as a percentage of the total number of leukocytes. This parameter reflects a high RNA content cells, such as activated cells i.e. B lymphocytes secreting antibodies or plasma cells. The Sysmex analyzer can also detect the presence of circulating abnormal cells and trigger morphological flags such as abnormal lymphocytes or blasts flag (AbnLym/BL) as well as abnormal scattergram (abnormal scatter).In our study, the analyzer operated in routine mode according to the manufacturer’s instructions. Three levels of internal quality controls were regularly evaluated. Numerical data and qualitative flags were recorded and studied for all samples.
Morphological study
Blood films were prepared and stained with May-Grünwald Giemsa staining. Smears were reviewed for cytological features by an expert hematologist who was blind to patients’ demographics and clinical information. Samples exhibiting nucleated red blood cells were excluded from the study. The evaluated morphological criterion was the presence of atypical lymphocytes and smudge cells.
Population data and diagnostic criteria
Patients’ demographic, clinical and laboratory data were obtained from medical records. Two groups of CL and RL were formed. The clonal origin of lymphocytosis was confirmed by flow cytometry and/or histological data (if bone marrow biopsy had been performed). In the CL group, all patients were diagnosed within the two years preceding the study and were not on chemotherapy at the time of sample collection. The reactive origin of lymphocytosis was defined as a decrease in lymphocytosis during hospitalization or the demonstration of clinical or biological pattern showing recent infection.
Statistical analysis
All data were analyzed with the SPSS 19.0 software. The Shapiro-Wilk test was used to determine normal distribution of continuous variables. Unpaired Student t-test was used to compare age and absolute lymphocytes count between the two groups. The Mann-Whitney U test was used to compare other continuous variables. Qualitative morphological flags were compared using the Fisher exact test. Receiver operating characteristic (ROC) curves were generated. The areas under the curve (AUC) were analyzed and values above 0.7 indicated favorable diagnostic accuracy. Discriminatory parameters, optimal cut-offs, sensitivity and specificity were established using the ROC curve analysis. The accuracy was calculated by 2 × 2 truth tables as follows: Accuracy = (true negative + true positive)/(true negative + true positive + false negative+ false positive). A p-value of < 0.05 was considered statistically significant.
Ethical considerations
This study was carried out on routine samples collected for diagnostic procedures. Parameters were obtained without any additional cost and without compromising the results of the clinical analysis. The study protocol was in accordance with the Declaration of Helsinki. The ethical clearance for this study was obtained from the local institutional review board.
RESULTS
General characteristics of the subjects
Ninety samples (lymphocytosis> 5G/L) from 67 patients were collected during the study period. Five samples were excluded because of interference due to the presence of nucleated red blood cells in the blood films. Overall, 85 samples were divided into two groups of CL (n=51) and RL (n=34).There were 38 cases of chronic lymphocytic leukemia (CLL), 12 cases of LPD non-CLL and one case of acute lymphoblastic leukemia. Demographic characteristics and extended CBC findings of the two groups are presented in table1.
Table 1.Comparative analysis of clinical and hematological parameters in CL and RL groups
| Variable | Clonal Lymphocytosis | Reactive Lymphocytosis | P-value |
| Age (years) | 71,43 ±10 ,67 | 49,69 ±14,2 | <10-3 |
| Gender (Male/Female) | 24/27 | 17/17 | 0.827 |
| WBC (G/l) | 54.388 ± 4. 898 | 14.022 ±3.377 | <10-3 |
| Absolute Lymphocytes (G/l) | 46.478 ± 46.341 | 5.916 ± 1.063 | <10-3 |
| Neutrophils (G/l) | 4.191 ± 2.990 | 6.531 ±2.789 | <10-3 |
| Eosinophils (G/l) | 237.45 ± 305 | 302.65± 282.32 | 0.316 |
| Basophils (G/l) | 90.1 ± 39 | 89.41 ± 16 | 0.4 |
| HFLC (%) | 0.049 ± 0.11 | 0.153 ± 0.267 | 0.01 |
| IG (%) | 0.3 ± 0.39 | 0.54 ± 0.89 | 0.1 |
| RBC (106/μl) | 3.74 ± 0.09 | 4.64 ± 0.08 | <10-3 |
| Hemoglobin (g/dl) | 10.76 ± 2.7 | 12.8 ± 2.46 | 10-3 |
| MCV (fl) | 90.71 ± 11.89 | 84.14 ± 12.44 | <10-3 |
| MCH (pg) | 28.97 ± 3.89 | 27.97 ± 4.64 | 0.28 |
| RDW (%) | 16.05 ± 2.64 | 15.32 ± 2.46 | 0.2 |
| Platelets (G/l) | 209.961 ± 201.787 | 381.735 ± 152.904 | <10-3 |
Data are presented as mean ± standard deviation. [1] WBC: white blood cells, HFLC : High fluorescence lymphocyte, IG : immature granulocytes, RBC : red blood cells, MCV : mean corpuscular volume, MCH: mean corpuscular hemoglobin, RDW : red distribution width, SD standard deviation
P-values in bold italics are statistically significant (<0.05)
Absolute lymphocytes count ranged from 6.92 to 173.11G/l in the CL group and from 5 to 9.93G/l in the RL group.
ROC curves analysis
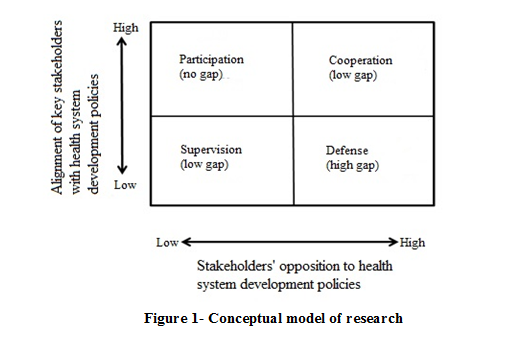
The ROC, AUC and related data are displayed in table 2. The results showed that WBC, ALC and patient’s age allowed excellent discrimination between CL and RL (Figure 1).
Table 2.Performance of the discriminating parameters between clonal and reactive lymphocytosis and determination of their cut-offs
P-values in bold italics are statistically significant (<0.05)
Absolute lymphocytes count ranged from 6.92 to 173.11G/l in the CL group and from 5 to 9.93G/l in the RL group.
ROC curves analysis
The ROC, AUC and related data are displayed in table 2. The results showed that WBC, ALC and patient’s age allowed excellent discrimination between CL and RL (Figure 1).
Table 2.Performance of the discriminating parameters between clonal and reactive lymphocytosis and determination of their cut-offs
| AUC | 95% confidence interval | p-value | Cut-off | Sensitivity | Specificity | Accuracy | |
| Age (years) | 0.9 | [0.834-0.97] | <10-3 | 62.5 | 74.5% | 82.4% | 80.3% |
| Lymphocytes (G/l) | 0.99 | [0.983- 1] | <10-3 | 10.47 | 96.7% | 100% | 96% |
| WBC (G/l) | 0.94 | [0.893- 0.994] | <10-3 | 17.745 | 88% | 85.3% | 92.15% |
| Neutrophils (G/l) | 0.74 | [0.642- 0.854] | <10-3 | 4.87 | 70% | 76.5% | 74.5% |
| HFCL % | 0.71 | [0.6- 0.829] | 10-3 | 0.05 | 76.5% | 67.6% | 76.5% |
| Hemoglobin (g/dl) | 0.70 | [0.593- 0.816] | 10-3 | 11.45 | 69% | 77% | 75.1% |
| Platelets (G/l) | 0.83 | [0.739- 0.924] | <10-3 | 242.5 | 74.5% | 82.4% | 80.4% |
P-value, in bold indicates a significant difference (<0.05)
.PNG)
Morphological flags assessment
The ‘’AbnLym/BL’’ and ‘’abnormal scatter’’ flags showed a statistically significant association with CL status, while ‘’AbnLym/BL’’ demonstrated high positive likelihood ratio of 14.97.
Contribution of cytological study in the distinction between RL and CL
Observation of atypical lymphocytes in the blood smears was significantly associated with RL (p=10-3). However, presence of smudge cells was suggestive of CL diagnosis (p=10-3).
Proposal of an algorithm based on clinical and extended CBC parameters
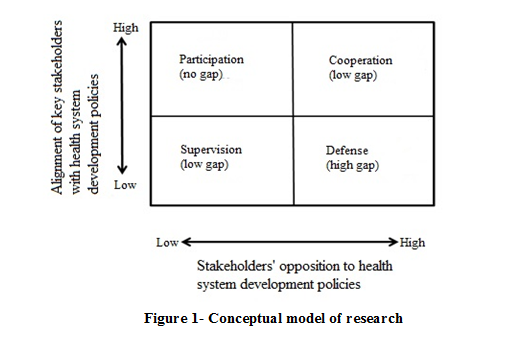
The results showed that age, lymphocyte count, HFLC% and the ’’AbnLym/Bl’’ flag were predictor of CL. Therefore, we proposed the following strategy to detect CL: for ALCof >10.47 g/l, a blood smear is immediately necessary regardless of the patient’s age. When a CL morphology is suspected, a flow cytometry is indicated. In case of inconclusive blood smear, the integration of clinical information such as chronic lymphocytosis, presence of splenomegaly or adenomegaly, a remote check of the blood count and blood smear are necessary to decide a flow cytometric analysis. For moderate lymphocytosis between 5 G/l and 10.47 G/l, a blood smear is performed. If the morphological examination does not distinguish RC from malignant lymphocytosis, an age-based orientation is proposed. For patients older than 62.5years, clinical information is required in order to decide whether a flow cytometry is indicated or only a closer control of the blood count is appropriate. For patients older than 62.5 years with HFLC% <0.05% regardless the ’AbnLym/Bl’’ flagging a flow cytometry is indicated. However, in case of HFLC% >0.05% without flagging, a follow-up with CBC and blood smears are proposed. When ‘’AbnLym/Bl’’ is present, patients are likely to harbor LPD and a flow cytometry should be considered (Figure 2).
When the malignant morphology is found in the blood smear examination, a flow cytometry is suggested. In case of reactive morphology, a short follow-up of patients with remote control of ALC and blood films is proposed. The application of the ALC threshold of 10.47 G/l alone to our pool of cases showed a high ability to identify CL achieving a sensitivity of 96.7% and a specificity of 100 %. Moreover, when considering both the ALC range of 5-10.47G/l and age of 62.5 years old, there were no false positive or negative results detected.
DISCUSSION
Rapid differentiation of malignant lymphocytosis from RL is critical for proper patient management. The ISLH recommends the analysis of blood smears as a first-line examination when discovered a blood lymphocytosis of more than 5 G/l (4). However, the cytological examination has its limits and could be inconclusive. A review of recent literature has shown interest in using available research parameters and morphological flags on hematology analyzers to optimize the etiological orientation of lymphocytosis and to save time (11-13). The pertinence of considering patients’ age for malignant lymphocytosis screening was also reported (11). In this study, we assessed the relevance of searching for parameters that may be helpful to discriminate CL from RL.
According to our data, advanced age, leukocytosis and lymphocytosis as well as low HFLC were predictive of malignant lymphocytosis. Despite the small sample size due to non-inclusion of samples from the emergency department, the majority of our results were consistent with those of the literature. Sun et al. reported a median age of 66 years old (range: 47–91 years) in CL group and 52 years (range: 19–90 years) in RL group (10). In our study, an age cut-off of 62.5 years showed an AUC of 0.9 with an accuracy of 80.3%. Other studies reported an age threshold of between 50 and 67 years old (11,13,14). A study in France established a cut-off of 60 years with good performance (AUC= 0.875; 95% confidence interval: [0.831- 0.918]; p=10-3, sensitivity: 83.5%, specificity: 75.6%) (6).
The best cut-off value of ALC in our study was 10.47 G/l showing an accuracy of 96%. Andrews et al. suggested a threshold of 4 G/l for patients over the age of 67 years and > 6.7G/l for patients aged 50 to 67 years (11).In the study by Sun et al., the optimal cut-off was about 7G/l (AUC= 0.8894) (10). A previous study in Italy proposed the threshold of 10G/lB-lymphocytes for predicting CLL (15).However, the same threshold was also reported by Tseng but with poor sensitivity (AUC: 0.732; sensitivity: 52%) (13). Currently, the 5G/l lymphocytes cut-off recommended by the ISLH is widely adopted by many hematology laboratories as a trigger for a cytological review (4), but it could be more reasonable to include the age and ALC cut-offs than lymphocytosis alone (10, 11). According to Tseng et al., for cases with lymphocytosis between 5 and 10 G/l, age was used as a discriminatory parameter (AUC of 0.886) and on the selection of patients over 50 years of age, this approach made it possible to direct the diagnosis towards a CL with a sensitivity of 93% and a specificity of 62%. When applied to a validation cohort, the performance of the thresholds was maintained while reducing smears review by 50% (13).
As mentioned earlier, the HFLC parameter indicates the presence of high fluorescence cells, reflecting a high RNA content corresponding to activated lymphocytes (T-cells), plasma cells, large granular lymphocytes or natural killer cells (8, 16). These cells are often found in reactive conditions but could be observed during LPD in a smaller proportion. As expected, the association of HFLC% with reactive lymphocytosis was demonstrated and provided an AUC of 0.71.Values below 0.05% showed a sensitivity of 76.5% and a specificity of 67.6%. A lack of sensitivity of the HFLC % was also reported in another study (6). It is important to notice that, in general, the search parameters depend on the hematology analyzer and do not have a specific reference range or external quality assurance. All these reasons could explain why the HFLC parameter is not commonly used in routine laboratories.
Among the qualitative flags generated by the Sysmex XT 4000i® analyzer, we demonstrated a significant association between the ‘AbnLym/Bl’ flag and the CL group with high performance levels. Similar results were reported in other studies (6, 16). Furthermore, Brisou et al. demonstrated the reliability of the combination of ‘AbnLym/Bl’ flag and some structural lymphocyte parameters for defining blood slide review to screen circulating Sezary cells and B-cell diseases (17).
In keeping with the recommendations of the ISLH/GFHC (blood smear for lymphocytosis greater than 5G/l), we tried to refine the approach according to the lymphocyte count by integrating the study cut-offs (10.47 G/l for ALC and age of 62.5 years). The threshold ALC of 10.47 G/l had 100% specificity for LPD. Performance of different thresholds adopted by other studies did not reach such specificity (6, 10, 13). But for moderate lymphocytosis with ALC range between 5G/l and 10.47G/l, the distinction between CL and RL may not be easy. In fact, this situation is frequent in our practice, and paradoxically guidelines are still not well-defined. Our proposed approach for moderate lymphocytosis is especially useful when the blood smear is not conclusive. With the combination of age threshold, no true or false positive was noticed. In some studies, the combination of these two parameters also showed encouraging results with a sensitivity of 93.8 % and a specificity of 80.8%(6, 10).However, different approaches based on the use of the lymphocyte positional parameters (other extended CBC parameters) regardless of the patients’ age, may be beneficial for a routine laboratory identification of clonal lymphocyte proliferation (12, 16).
In our study, we also proposed to use the HFLC% and the ''AbnLym/Bl' alarm. These parameters are available on hematology analyzers without additional cost and could be useful to help provide guidance for clinical hematology practice in cases of moderate lymphocytosis. However, these results should be interpreted with caution regarding the relative small sample size and the lack of a validation cohort.
CONCLUSION
In an era of evidence-based medicine, it is important to establish specific criteria to guide decision toward peripheral blood lymphocytosis. This study emphasized the usefulness of considering the ALC and age thresholds as first line orientation, especially in moderate lymphocytosis. The clinical application of combining clinical data, extended CBC parameters and morphological flags for discriminating CL and RL merits further investigation.
ACKNOWLEDGMENTS
None.
DECLARATIONS
Funding
The authors received no financial support for this study.
Ethics approvals and consent to participate
The study protocol was in accordance with the Declaration of Helsinki. The ethical clearance for the study was obtained from the local institutional review board.
Conflicts of interest
The authors declare that there is no conflict of interest.
.PNG)
Morphological flags assessment
The ‘’AbnLym/BL’’ and ‘’abnormal scatter’’ flags showed a statistically significant association with CL status, while ‘’AbnLym/BL’’ demonstrated high positive likelihood ratio of 14.97.
Contribution of cytological study in the distinction between RL and CL
Observation of atypical lymphocytes in the blood smears was significantly associated with RL (p=10-3). However, presence of smudge cells was suggestive of CL diagnosis (p=10-3).
Proposal of an algorithm based on clinical and extended CBC parameters
The results showed that age, lymphocyte count, HFLC% and the ’’AbnLym/Bl’’ flag were predictor of CL. Therefore, we proposed the following strategy to detect CL: for ALCof >10.47 g/l, a blood smear is immediately necessary regardless of the patient’s age. When a CL morphology is suspected, a flow cytometry is indicated. In case of inconclusive blood smear, the integration of clinical information such as chronic lymphocytosis, presence of splenomegaly or adenomegaly, a remote check of the blood count and blood smear are necessary to decide a flow cytometric analysis. For moderate lymphocytosis between 5 G/l and 10.47 G/l, a blood smear is performed. If the morphological examination does not distinguish RC from malignant lymphocytosis, an age-based orientation is proposed. For patients older than 62.5years, clinical information is required in order to decide whether a flow cytometry is indicated or only a closer control of the blood count is appropriate. For patients older than 62.5 years with HFLC% <0.05% regardless the ’AbnLym/Bl’’ flagging a flow cytometry is indicated. However, in case of HFLC% >0.05% without flagging, a follow-up with CBC and blood smears are proposed. When ‘’AbnLym/Bl’’ is present, patients are likely to harbor LPD and a flow cytometry should be considered (Figure 2).
When the malignant morphology is found in the blood smear examination, a flow cytometry is suggested. In case of reactive morphology, a short follow-up of patients with remote control of ALC and blood films is proposed. The application of the ALC threshold of 10.47 G/l alone to our pool of cases showed a high ability to identify CL achieving a sensitivity of 96.7% and a specificity of 100 %. Moreover, when considering both the ALC range of 5-10.47G/l and age of 62.5 years old, there were no false positive or negative results detected.
DISCUSSION
Rapid differentiation of malignant lymphocytosis from RL is critical for proper patient management. The ISLH recommends the analysis of blood smears as a first-line examination when discovered a blood lymphocytosis of more than 5 G/l (4). However, the cytological examination has its limits and could be inconclusive. A review of recent literature has shown interest in using available research parameters and morphological flags on hematology analyzers to optimize the etiological orientation of lymphocytosis and to save time (11-13). The pertinence of considering patients’ age for malignant lymphocytosis screening was also reported (11). In this study, we assessed the relevance of searching for parameters that may be helpful to discriminate CL from RL.
According to our data, advanced age, leukocytosis and lymphocytosis as well as low HFLC were predictive of malignant lymphocytosis. Despite the small sample size due to non-inclusion of samples from the emergency department, the majority of our results were consistent with those of the literature. Sun et al. reported a median age of 66 years old (range: 47–91 years) in CL group and 52 years (range: 19–90 years) in RL group (10). In our study, an age cut-off of 62.5 years showed an AUC of 0.9 with an accuracy of 80.3%. Other studies reported an age threshold of between 50 and 67 years old (11,13,14). A study in France established a cut-off of 60 years with good performance (AUC= 0.875; 95% confidence interval: [0.831- 0.918]; p=10-3, sensitivity: 83.5%, specificity: 75.6%) (6).
The best cut-off value of ALC in our study was 10.47 G/l showing an accuracy of 96%. Andrews et al. suggested a threshold of 4 G/l for patients over the age of 67 years and > 6.7G/l for patients aged 50 to 67 years (11).In the study by Sun et al., the optimal cut-off was about 7G/l (AUC= 0.8894) (10). A previous study in Italy proposed the threshold of 10G/lB-lymphocytes for predicting CLL (15).However, the same threshold was also reported by Tseng but with poor sensitivity (AUC: 0.732; sensitivity: 52%) (13). Currently, the 5G/l lymphocytes cut-off recommended by the ISLH is widely adopted by many hematology laboratories as a trigger for a cytological review (4), but it could be more reasonable to include the age and ALC cut-offs than lymphocytosis alone (10, 11). According to Tseng et al., for cases with lymphocytosis between 5 and 10 G/l, age was used as a discriminatory parameter (AUC of 0.886) and on the selection of patients over 50 years of age, this approach made it possible to direct the diagnosis towards a CL with a sensitivity of 93% and a specificity of 62%. When applied to a validation cohort, the performance of the thresholds was maintained while reducing smears review by 50% (13).
As mentioned earlier, the HFLC parameter indicates the presence of high fluorescence cells, reflecting a high RNA content corresponding to activated lymphocytes (T-cells), plasma cells, large granular lymphocytes or natural killer cells (8, 16). These cells are often found in reactive conditions but could be observed during LPD in a smaller proportion. As expected, the association of HFLC% with reactive lymphocytosis was demonstrated and provided an AUC of 0.71.Values below 0.05% showed a sensitivity of 76.5% and a specificity of 67.6%. A lack of sensitivity of the HFLC % was also reported in another study (6). It is important to notice that, in general, the search parameters depend on the hematology analyzer and do not have a specific reference range or external quality assurance. All these reasons could explain why the HFLC parameter is not commonly used in routine laboratories.
Among the qualitative flags generated by the Sysmex XT 4000i® analyzer, we demonstrated a significant association between the ‘AbnLym/Bl’ flag and the CL group with high performance levels. Similar results were reported in other studies (6, 16). Furthermore, Brisou et al. demonstrated the reliability of the combination of ‘AbnLym/Bl’ flag and some structural lymphocyte parameters for defining blood slide review to screen circulating Sezary cells and B-cell diseases (17).
In keeping with the recommendations of the ISLH/GFHC (blood smear for lymphocytosis greater than 5G/l), we tried to refine the approach according to the lymphocyte count by integrating the study cut-offs (10.47 G/l for ALC and age of 62.5 years). The threshold ALC of 10.47 G/l had 100% specificity for LPD. Performance of different thresholds adopted by other studies did not reach such specificity (6, 10, 13). But for moderate lymphocytosis with ALC range between 5G/l and 10.47G/l, the distinction between CL and RL may not be easy. In fact, this situation is frequent in our practice, and paradoxically guidelines are still not well-defined. Our proposed approach for moderate lymphocytosis is especially useful when the blood smear is not conclusive. With the combination of age threshold, no true or false positive was noticed. In some studies, the combination of these two parameters also showed encouraging results with a sensitivity of 93.8 % and a specificity of 80.8%(6, 10).However, different approaches based on the use of the lymphocyte positional parameters (other extended CBC parameters) regardless of the patients’ age, may be beneficial for a routine laboratory identification of clonal lymphocyte proliferation (12, 16).
In our study, we also proposed to use the HFLC% and the ''AbnLym/Bl' alarm. These parameters are available on hematology analyzers without additional cost and could be useful to help provide guidance for clinical hematology practice in cases of moderate lymphocytosis. However, these results should be interpreted with caution regarding the relative small sample size and the lack of a validation cohort.
CONCLUSION
In an era of evidence-based medicine, it is important to establish specific criteria to guide decision toward peripheral blood lymphocytosis. This study emphasized the usefulness of considering the ALC and age thresholds as first line orientation, especially in moderate lymphocytosis. The clinical application of combining clinical data, extended CBC parameters and morphological flags for discriminating CL and RL merits further investigation.
ACKNOWLEDGMENTS
None.
DECLARATIONS
Funding
The authors received no financial support for this study.
Ethics approvals and consent to participate
The study protocol was in accordance with the Declaration of Helsinki. The ethical clearance for the study was obtained from the local institutional review board.
Conflicts of interest
The authors declare that there is no conflict of interest.
Research Article: Original Paper |
Subject:
Laboratory hematology
Received: 2021/07/27 | Accepted: 2021/08/30 | Published: 2021/10/18 | ePublished: 2021/10/18
Received: 2021/07/27 | Accepted: 2021/08/30 | Published: 2021/10/18 | ePublished: 2021/10/18
References
1. Shiftan TA, Mendelsohn J. The circulating "atypical" lymphocyte. Human Pathology. 1978; 9(1): 51-61. [View at Publisher] [DOI:10.1016/S0046-8177(78)80007-0] [PubMed] [Google Scholar]
2. Macintyre EA, Linch DC. Lymphocytosis is it leukaemia and when to treat. Postgraduate Medical Journal. 1988; 64(747): 42-7. [View at Publisher] [DOI:10.1136/pgmj.64.747.42] [PubMed] [Google Scholar]
3. Swerdlow SH, Campo E, Pileri SA, Lee Harris N, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization (WHO) classification of lymphoid neoplasms. Blood. 2016; 127(20): 2375-90. [View at Publisher] [DOI:10.1182/blood-2016-01-643569] [PubMed] [Google Scholar]
4. Barnes PW, McFadden SL, Machin SJ, Simson E. The international consensus group for hematology review: suggested criteria for action following automated CBC and WBC differential analysis. Lab Hematol . 2005; 11(2): 83-90. [DOI:10.1532/LH96.05019] [PubMed] [Google Scholar]
5. Genevieve F, Galoisy AC, Bataille DM, Wagner-Ballon O, Trimoreau F, Fenneteau O, et al. Revue microscopique du frottissanguin : proposition du groupe Francophone d'hematologiecellulaire. Feuillets de Biologie. 2014;317:2-16. [View at Publisher]
6. Rose Johann. Hyperlymphocytose sanguine modérée de l'adulte :Seuilsrationnels et orientation optimale au laboratoired'hématologie [thesis]. Départementd'hématologieetd'immunologie: Angers. 2016; 53. [View at Publisher] [Google Scholar]
7. George TI. Malignant or benign leukocytosis. Hematology Am SocHematolEduc Program. 2012;2012:475-84. [DOI:10.1182/asheducation.V2012.1.475.3798515] [PubMed] [Google Scholar]
8. ChaicharoenTantanate, CherdsakKlinbua. Performance Evaluation of High Fluorescence Lymphocyte Count: Comparability to Atypical Lymphocyte Count and Clinical Significance. Laboratory Medicine 2018;49(4):362-368. doi: 10.1093/labmed/lmy030. [View at Publisher] [DOI:10.1093/labmed/lmy030] [PubMed] [Google Scholar]
9. Seghezzi M, Buoro S, Previtali G, Moioli V, Manenti B, Simon-Lopez R et al. A preliminary proposal for quality control assessement and harmonizaton for leucocytes morphology.Structural parameters (Cell population data parameters).Journal of Medical biochemistry. 2018;37(4):486-98.doi: 10.2478/jomb-2018-0005 [DOI:10.2478/jomb-2018-0005] [PubMed] [Google Scholar]
10. Sun P, Kowalski EM, Cheng CK, Shawwa A, Liwski RS, Juskevicius R. Predictive significance of absolute lymphocyte count and morphology in adults with a new onset peripheral blood lymphocytosis. Journal of Clinical Pathology. 2014; 67(12): 1062-6. [DOI:10.1136/jclinpath-2014-202545] [PubMed] [Google Scholar]
11. Andrews JM, Cruser DL, Myers JB, Fernelius CA, Holm MT, Waldner DL. Using peripheral smear review, age and absolute lymphocyte count as predictors of abnormal peripheral blood lymphocytoses diagnosed by flow cytometry. Leuk Lymphoma. 2008; 49(9): 1731-7. [View at Publisher] [DOI:10.1080/10428190802251787] [PubMed] [Google Scholar]
12. Jean A, Boutet C, Lenormand B, Callat MP, Buchonnet G, Leclerc C, et al. Combination of cellular population data and CytoDiffTM analyses for the diagnosis of lymphocytosis. Clinical Chemistryand Laboratory Medicine. 2011; 49(11): 1861-1868. [View at Publisher] [DOI:10.1515/cclm.2011.680] [PubMed] [Google Scholar]
13. Tseng V, Morgan AS, Leith CP, Yang DT. Efficient assessment of peripheral blood lymphocytosis in adults: developing new thresholds for blood smear review by pathologists. Clinical Chemistry and Laboratory Medicine 2014; 52(12): 1763-1770. [View at Publisher] [DOI:10.1515/cclm-2014-0320] [PubMed] [Google Scholar]
14. Oberley MJ, Fitzgerald S, Yang DT, Morgan A, Johnson J, Leith C. Value-based flow testing of chronic lymphoproliferative disorders: a quality improvement project to develop an algorithm to streamline testing and reduce costs. American Journal of Clinical Pathology. 2014; 142(3): 411-8. [View at Publisher] [DOI:10.1309/AJCP0SWZJ6GBDHPF] [PubMed] [Google Scholar]
15. Molica S, Mauro FR, Giannarelli D, Lauria F, Cortelezzi A, Brugiatelli M et al. Differentiating chronic lymphocytic leukemia from monoclonal B-lymphocytosis according to clinical outcome: on behalf of the GIMEMA chronic lymphoproliferative diseases working group. Haematologica. 2011; 96(2): 277-83.
https://doi.org/10.3324/haematol.2010.030189 [View at Publisher] [DOI:10.3324/haematol.2010.030189.] [PubMed] [Google Scholar]
16. Xie H, Wu Y, Cui W. Correlation between the cell population in the automated hematology analyzer high-fluorescence region and atypical lymphocyte flags. Journal of Clinical Laboratory Analysis. 2018;32(5):e22374. doi: 10.1002/jcla.22374. [View at Publisher] [DOI:10.1002/jcla.22374] [PubMed] [Google Scholar]
17. Brisou G, Manzoni D, Dalle S, Felman P, Morel D, Boubaya M, et al. Alarms and parameters generated by hematology analyzer: new tools to predict and quantify circulating Sezary cells. Journal of Clinical Laboratory Analysis. 2015;29(2):153 61. doi: 10.1002/jcla.21744 [View at Publisher] [DOI:10.1002/jcla.21744] [PubMed] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.







