Volume 17, Issue 6 (Nov-Dec 2023)
mljgoums 2023, 17(6): 8-9 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezanezhadi M, Azadi F, Marhamati S, Joshaghani H R. Rapid and direct detection of herpes simplex virus type 1 and type 2 by Real-Time PCR
method in clinical specimens. mljgoums 2023; 17 (6) :8-9
URL: http://mlj.goums.ac.ir/article-1-1334-en.html
URL: http://mlj.goums.ac.ir/article-1-1334-en.html
1- Kavosh Medical Laboratory, Research and Development Unit, Gorgan, Iran
2- . Department of Microbiology, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran. Laboratory Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- Department of Biochemistry, Golestan University of Medical Sciences, Gorgan, Iran
4- Laboratory Research Center, Golestan University of Medical Sciences, Gorgan, Iran , hr_joshaghani@yahoo.com
2- . Department of Microbiology, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran. Laboratory Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- Department of Biochemistry, Golestan University of Medical Sciences, Gorgan, Iran
4- Laboratory Research Center, Golestan University of Medical Sciences, Gorgan, Iran , hr_joshaghani@yahoo.com
Full-Text [PDF 281 kb]
(112 Downloads)
| Abstract (HTML) (411 Views)
Full-Text: (67 Views)
Introduction
Human Herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2) are members of the Herpesviridae family (1) surrounded by DNA viruses that are susceptible to disinfectants and environmental agents (2). Due to genetic homology between HSV-1 and HSV-2, numerous biological similarities and antigenic cross-reactions exist between these two viruses (3). HSV-1 and HSV-2 are responsible for a broad range of human diseases worldwide, including oral and genital mucosal lesions and encephalitis (1,4).
Following primary infection, HSV-1 and HSV-2 have the capacity to stay latent in the nerve ganglia (4) and are triggered by some factors such as fever, stress, and trauma (2). In certain cases, primary infection or reactivation of HSV viruses can lead to central nervous system (CNS) diseases (5). HSV-1 is responsible for nearly 10 % of cases of encephalitis and is the most frequent cause of fatal sporadic viral encephalitis worldwide (6, 7). The HSV-1 encephalitis (HSE) mortality risk can be higher than 70% if left untreated (7). HSV-2 infection can lead to meningitis (4,6) or meningoencephalitis, which can recur after treatment. HSV-2 can also cause diffuse infections in 25% of infants (4).
Primary genital infections with HSV-1 and HSV-2 are typically asymptomatic (8). Clinical symptoms typically begin with the emergence of macules and papules on the skin and mucous membranes and develop into ulcers after about 3 weeks. The transmission of HSV-1 and HSV-2 is made by direct contact. Primary HSV-1 infection also occurs in infancy after the disappearance of maternal antibodies in the first year of life. According to research undertaken in Germany, there is a strong association between aging and an increase in IgG anti-HSV-1 titer, the frequency of which is 85-90% for HSV-1 in adults over 40 years of age. However, HSV-2 is predominantly sexually transmitted. It can be seen after puberty in people who have multiple sexual partners and in homosexual men (2).
As there is typically no treatment for latent infection, appropriate treatment requires a test that can easily diagnose the infection. The specificity of the test is also very important, as clinical manifestations of HSV can overlap with other infections. It should also be a measure that can be applicable to several clinical specimens (1). The methods recently used as an alternative to cell culture and serological methods are molecular methods with advantages such as rapid access to data, usefulness for a range of clinical specimens, and high sensitivity and specificity (6,9). Since the central nervous system infection due to HSV is a medical emergency that can lead to high morbidity and mortality, rapid diagnosis and initiation of therapy are crucial (4). The identification of HSV-1 and HSV-2 in the cerebrospinal fluid (CSF) using RT-PCR for the diagnosis of HSV and herpes meningitis is now known as the gold standard (10). A variety of RT-PCR experiments have been found to be more sensitive and specific (>95%) in detecting and distinguishing HSV-1 and HSV-2 relative to the cell culture (4). Therefore, we planned to detect Herpes viruses in this project using the RT-PCR process.
Methods
In this cross-sectional study, 645 patients hospitalized in health centers of Golestan Province, Iran, suspected of having HSV infection were selected during 2015 and 2020. All the patients gave their informed consent and participated on a voluntary basis. Demographic data (sex and age) and samples were obtained. Specimens were sent to the Gorgan Kavosh Laboratory, and the identification of HSV-1 and HSV-2 on the samples obtained over a 5-year period was conducted using the RT-PCR. The samples contained CSF (593 cases), serum (41 cases), vaginal, pleural fluid, bronchoalveolar lavage, pericardium, ulcer, and plasma (11 cases).
The HSV DNA was extracted from 200-μL samples using the High Pure PCR Template Preparation Kit (Roche Diagnostics®, Mannheim, Germany) according to the manufacturer's protocol.
PCR was performed for HSV with the Geneproof Kit (Geneproof Herpes Simplex Virus (HSV-1/2) PCR Kit, Taiwan). Briefly, 10 µL of the extracted DNA was applied to 30 µL of the master mix in the PCR tubes. The amplification was performed under the following thermal conditions: incubation at 37 °C for 2 min, 95 °C for 10 min, and 45 cycles consisting of denaturation at 95 °C for 5 s, annealing at 60 °C for 40 s, and extension at 72 °C for 20 s.
Results
In this study, a total of 645 patient samples were analysed, include 291 females (45.1%) and 354 males (54.8%). Patients age were from 1 months to 96 years. The samples were included Cerebrospinal fluid (CSF) (593 cases), serum (41cases) and 11 cases of (Vaginal, Pleural fluid, bronchoalveolar lavage, pericard, ulcer and Plasma). Of the 645 samples tested by RT-PCR, 9 samples (1.39 %) were detected to be positive, and 636 samples (98.6 %) were found to be negative. Of the positive samples, 8 cases (88.8%) were HSV-1 and 1case (11.1%) was HSV-2. Among the positive samples of HSV-1, 7 cases (77.7%) were from CSF and 1 case (12.5%) of Vaginal which is probably due to genetic homology between the two viruses. HSV-2 were seen only in 1 vaginal specimen (11.1%). Also, of all positive specimens, 8 cases (88.8%) were female and 1 case (11.1%) was male. These results also are shown in (Table 1).
Discussion
Herpes simplex viruses type 1 (HSV-1) and type 2 (HSV-2) are widespread causes of different clinical presentation types, from skin vesicles to disseminated viral infection. Early diagnosis of these viral infections is very important as it can lead to early treatment and reduce further infection and even death. Various types of laboratory procedures have been used to diagnose this infection, including cell culture, which is considered a gold standard but also has limitations in processing time, physical labor, and loss of sensitivity (11). Serological tests that only indicate previous exposure to HSV-1 and HSV-2 are also not successful in the diagnosis of acute infection. Sensitive and reliable methods for detecting and identifying HSV-1 and HSV-2 infections are critical (1). Polymerase chain reaction can be used to diagnose HSV infections (12). Among the PCR methods, the RT-PCR assay has been shown to be more sensitive and specific (>95%) in identifying and differentiating HSV-1 and HSV-2 compared to cell culture (4). Thus, in the present study, the RT-PCR assay was used for rapid diagnosis of HSV in patients hospitalized in Golestan Province health centers.
Of all HSV specimens, 9 samples (1.39%) were found to be positive, 8 of which (88.8%) were HSV-1 and 1 was HSV-2. Among these positive samples, the samples with the highest percentage were CSF (77.7%), and most of the positive cases were female (88.8%). It was also observed that 1 positive sample (11.1%) of HSV-1 was from the vagina, which is probably due to genetic similarity and cross-reactivity between the two viruses. The age group of positive specimens ranged from 8 to 48 years. We found that the RT-PCR assay performs well in the identification of herpes virus, as is also stated by Binnicker et al. (4), who reported high sensitivity (96.2%) and specificity (97.9%) for the diagnosis of HSV-1 and HSV-2, respectively. Besides, in the study by Anderson et al. (1), the molecular approach was shown to have a sensitivity of 99.5% relative to cell culture. In Hong et al.'s study (11), however, virus isolation in the cell culture (considered the classic gold standard) had many limitations in the turnaround time, manual labor, and lack of sensitivity. According to Navidad et al. (13), the sensitivity and specificity of the molecular method to cell culture were observed. Samples stated to be positive for HSV-1 and HSV-2 by the cell culture method were negatively observed using the molecular method, and vice versa. Pormohammad et al.'s study (14) stated that RT-PCR was a successful test for the diagnosis of HSV-related meningitis. According to the meta-analysis performed by Malary et al. (15) in Iran, the prevalence (95% confidence intervals) of HSV-1, HSV-2, and total HSV among the Iranian population was 25.7%, 6.5%, and 42.04%, respectively.
It can also be inferred that the use of RT-PCR and melting curve analysis improved sensitivity and shortened time in the clinical samples. Accurate and less labor-intensive molecular assays in clinical laboratories can aid the rapid diagnosis and prompt treatment of patients.
Conclusion
Early diagnosis of these viral infections is very important as it can lead to early treatment and prevent further infection and even death. Direct diagnosis is recommended, and validated molecular assays are a good alternative to cell culture and serological methods due to improved sensitivity and specificity to identify and distinguish herpes types 1 and 2. Thus, it seems important to use molecular methods which can provide an incentive for rapid diagnosis and prompt therapeutic intervention. Therefore, this study recommends rapid and direct detection of Herpes simplex virus type 1 and type 2 by Real-time PCR in clinical specimens.
Acknowledgement
We are grateful to Golestan University of Medical Sciences, Science Research Center Laboratory, and Gorgan Kavosh Laboratory for supporting this study.
Funding sources
We are grateful to Gorgan Kavosh Laboratory for supporting this study.
Ethical statement
An informed consent was sought from patients after explaining the purpose of the research. The confidentiality and anonymity of the patients' data were assured. The study was authorized by the Ethical Committee of Golestan University of medical sciences, (Ethical code:ir.goums.rec.1400.268).
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Author contributions
All the authors have participated in one or more parts of the present study.
Masoomeh Rezanezhadi conducted the test. Fahimeh Azadi performed the data analysis and wrote the manuscript. Shayan Marhamati collected the data. Hamidreza Joshaghani supervised the project.
Human Herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2) are members of the Herpesviridae family (1) surrounded by DNA viruses that are susceptible to disinfectants and environmental agents (2). Due to genetic homology between HSV-1 and HSV-2, numerous biological similarities and antigenic cross-reactions exist between these two viruses (3). HSV-1 and HSV-2 are responsible for a broad range of human diseases worldwide, including oral and genital mucosal lesions and encephalitis (1,4).
Following primary infection, HSV-1 and HSV-2 have the capacity to stay latent in the nerve ganglia (4) and are triggered by some factors such as fever, stress, and trauma (2). In certain cases, primary infection or reactivation of HSV viruses can lead to central nervous system (CNS) diseases (5). HSV-1 is responsible for nearly 10 % of cases of encephalitis and is the most frequent cause of fatal sporadic viral encephalitis worldwide (6, 7). The HSV-1 encephalitis (HSE) mortality risk can be higher than 70% if left untreated (7). HSV-2 infection can lead to meningitis (4,6) or meningoencephalitis, which can recur after treatment. HSV-2 can also cause diffuse infections in 25% of infants (4).
Primary genital infections with HSV-1 and HSV-2 are typically asymptomatic (8). Clinical symptoms typically begin with the emergence of macules and papules on the skin and mucous membranes and develop into ulcers after about 3 weeks. The transmission of HSV-1 and HSV-2 is made by direct contact. Primary HSV-1 infection also occurs in infancy after the disappearance of maternal antibodies in the first year of life. According to research undertaken in Germany, there is a strong association between aging and an increase in IgG anti-HSV-1 titer, the frequency of which is 85-90% for HSV-1 in adults over 40 years of age. However, HSV-2 is predominantly sexually transmitted. It can be seen after puberty in people who have multiple sexual partners and in homosexual men (2).
As there is typically no treatment for latent infection, appropriate treatment requires a test that can easily diagnose the infection. The specificity of the test is also very important, as clinical manifestations of HSV can overlap with other infections. It should also be a measure that can be applicable to several clinical specimens (1). The methods recently used as an alternative to cell culture and serological methods are molecular methods with advantages such as rapid access to data, usefulness for a range of clinical specimens, and high sensitivity and specificity (6,9). Since the central nervous system infection due to HSV is a medical emergency that can lead to high morbidity and mortality, rapid diagnosis and initiation of therapy are crucial (4). The identification of HSV-1 and HSV-2 in the cerebrospinal fluid (CSF) using RT-PCR for the diagnosis of HSV and herpes meningitis is now known as the gold standard (10). A variety of RT-PCR experiments have been found to be more sensitive and specific (>95%) in detecting and distinguishing HSV-1 and HSV-2 relative to the cell culture (4). Therefore, we planned to detect Herpes viruses in this project using the RT-PCR process.
Methods
In this cross-sectional study, 645 patients hospitalized in health centers of Golestan Province, Iran, suspected of having HSV infection were selected during 2015 and 2020. All the patients gave their informed consent and participated on a voluntary basis. Demographic data (sex and age) and samples were obtained. Specimens were sent to the Gorgan Kavosh Laboratory, and the identification of HSV-1 and HSV-2 on the samples obtained over a 5-year period was conducted using the RT-PCR. The samples contained CSF (593 cases), serum (41 cases), vaginal, pleural fluid, bronchoalveolar lavage, pericardium, ulcer, and plasma (11 cases).
The HSV DNA was extracted from 200-μL samples using the High Pure PCR Template Preparation Kit (Roche Diagnostics®, Mannheim, Germany) according to the manufacturer's protocol.
PCR was performed for HSV with the Geneproof Kit (Geneproof Herpes Simplex Virus (HSV-1/2) PCR Kit, Taiwan). Briefly, 10 µL of the extracted DNA was applied to 30 µL of the master mix in the PCR tubes. The amplification was performed under the following thermal conditions: incubation at 37 °C for 2 min, 95 °C for 10 min, and 45 cycles consisting of denaturation at 95 °C for 5 s, annealing at 60 °C for 40 s, and extension at 72 °C for 20 s.
Results
In this study, a total of 645 patient samples were analysed, include 291 females (45.1%) and 354 males (54.8%). Patients age were from 1 months to 96 years. The samples were included Cerebrospinal fluid (CSF) (593 cases), serum (41cases) and 11 cases of (Vaginal, Pleural fluid, bronchoalveolar lavage, pericard, ulcer and Plasma). Of the 645 samples tested by RT-PCR, 9 samples (1.39 %) were detected to be positive, and 636 samples (98.6 %) were found to be negative. Of the positive samples, 8 cases (88.8%) were HSV-1 and 1case (11.1%) was HSV-2. Among the positive samples of HSV-1, 7 cases (77.7%) were from CSF and 1 case (12.5%) of Vaginal which is probably due to genetic homology between the two viruses. HSV-2 were seen only in 1 vaginal specimen (11.1%). Also, of all positive specimens, 8 cases (88.8%) were female and 1 case (11.1%) was male. These results also are shown in (Table 1).
Table 1. The frequency of herpes simplex virus (HSV) infection according to the kind of specimen and demographic data of HSV-suspected patients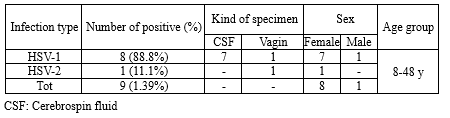 |
Discussion
Herpes simplex viruses type 1 (HSV-1) and type 2 (HSV-2) are widespread causes of different clinical presentation types, from skin vesicles to disseminated viral infection. Early diagnosis of these viral infections is very important as it can lead to early treatment and reduce further infection and even death. Various types of laboratory procedures have been used to diagnose this infection, including cell culture, which is considered a gold standard but also has limitations in processing time, physical labor, and loss of sensitivity (11). Serological tests that only indicate previous exposure to HSV-1 and HSV-2 are also not successful in the diagnosis of acute infection. Sensitive and reliable methods for detecting and identifying HSV-1 and HSV-2 infections are critical (1). Polymerase chain reaction can be used to diagnose HSV infections (12). Among the PCR methods, the RT-PCR assay has been shown to be more sensitive and specific (>95%) in identifying and differentiating HSV-1 and HSV-2 compared to cell culture (4). Thus, in the present study, the RT-PCR assay was used for rapid diagnosis of HSV in patients hospitalized in Golestan Province health centers.
Of all HSV specimens, 9 samples (1.39%) were found to be positive, 8 of which (88.8%) were HSV-1 and 1 was HSV-2. Among these positive samples, the samples with the highest percentage were CSF (77.7%), and most of the positive cases were female (88.8%). It was also observed that 1 positive sample (11.1%) of HSV-1 was from the vagina, which is probably due to genetic similarity and cross-reactivity between the two viruses. The age group of positive specimens ranged from 8 to 48 years. We found that the RT-PCR assay performs well in the identification of herpes virus, as is also stated by Binnicker et al. (4), who reported high sensitivity (96.2%) and specificity (97.9%) for the diagnosis of HSV-1 and HSV-2, respectively. Besides, in the study by Anderson et al. (1), the molecular approach was shown to have a sensitivity of 99.5% relative to cell culture. In Hong et al.'s study (11), however, virus isolation in the cell culture (considered the classic gold standard) had many limitations in the turnaround time, manual labor, and lack of sensitivity. According to Navidad et al. (13), the sensitivity and specificity of the molecular method to cell culture were observed. Samples stated to be positive for HSV-1 and HSV-2 by the cell culture method were negatively observed using the molecular method, and vice versa. Pormohammad et al.'s study (14) stated that RT-PCR was a successful test for the diagnosis of HSV-related meningitis. According to the meta-analysis performed by Malary et al. (15) in Iran, the prevalence (95% confidence intervals) of HSV-1, HSV-2, and total HSV among the Iranian population was 25.7%, 6.5%, and 42.04%, respectively.
It can also be inferred that the use of RT-PCR and melting curve analysis improved sensitivity and shortened time in the clinical samples. Accurate and less labor-intensive molecular assays in clinical laboratories can aid the rapid diagnosis and prompt treatment of patients.
Conclusion
Early diagnosis of these viral infections is very important as it can lead to early treatment and prevent further infection and even death. Direct diagnosis is recommended, and validated molecular assays are a good alternative to cell culture and serological methods due to improved sensitivity and specificity to identify and distinguish herpes types 1 and 2. Thus, it seems important to use molecular methods which can provide an incentive for rapid diagnosis and prompt therapeutic intervention. Therefore, this study recommends rapid and direct detection of Herpes simplex virus type 1 and type 2 by Real-time PCR in clinical specimens.
Acknowledgement
We are grateful to Golestan University of Medical Sciences, Science Research Center Laboratory, and Gorgan Kavosh Laboratory for supporting this study.
Funding sources
We are grateful to Gorgan Kavosh Laboratory for supporting this study.
Ethical statement
An informed consent was sought from patients after explaining the purpose of the research. The confidentiality and anonymity of the patients' data were assured. The study was authorized by the Ethical Committee of Golestan University of medical sciences, (Ethical code:ir.goums.rec.1400.268).
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Author contributions
All the authors have participated in one or more parts of the present study.
Masoomeh Rezanezhadi conducted the test. Fahimeh Azadi performed the data analysis and wrote the manuscript. Shayan Marhamati collected the data. Hamidreza Joshaghani supervised the project.
Research Article: Original Paper |
Subject:
Microbiology
Received: 2020/09/23 | Accepted: 2020/09/24 | Published: 2024/02/26 | ePublished: 2024/02/26
Received: 2020/09/23 | Accepted: 2020/09/24 | Published: 2024/02/26 | ePublished: 2024/02/26
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.







